Table of content
Diabetes, mother of all diseases, is an acute health condition that requires a multi-dimensional treatment approach. And if left untreated, this condition can create life-threatening complications. Diabetics and their caretakers or loved ones must have awareness of acute complications of diabetes and their symptoms. The experts of Cgm Monitors will tell you about acute complications of diabetes with their symptoms and precautions on the basis of real expertise and research, because your care starts here.
1. Diabetic Ketoacidosis (DKA)
The sugar from carbohydrates is a major source of your body’s energy. Without enough insulin, glucose can’t enter your cells for use. When your blood sugar stays high and your body doesn’t have enough insulin, it starts breaking down fats for energy. This produces ketones (acidic compounds), and if they build up in the blood, the condition is called Diabetic Ketoacidosis (DKA).
DKA mainly occurs in people with type 1 diabetes, but it can also affect people with type 2 diabetes during illness, severe insulin deficiency, or certain medication use.
Important: While the keto diet is popular today, it can be risky for people who do not produce enough insulin, such as those with type 1 diabetes. In these cases, ketosis can quickly turn into dangerous DKA.
Because people with type 1 diabetes depend on insulin, they are at the highest risk of experiencing DKA.
Symptoms:
- High blood sugar levels
- Dehydration in diabetes
- Fruity-smelling breath
- Rapid breathing
- Nausea and vomiting
- Altered mental status
Causes:
- Lack of insulin
- Illness or infection
- Stress or trauma
Prevention:
- Consistent insulin management
- Regular blood glucose monitoring
- Early treatment of infections or illnesses
- Staying hydrated to prevent dehydration in diabetes
Are you satisfied with fingerpricks?
Continuous glucose monitors (CGMs) like Freestyle Libre 2 Plus Sensors can help you with 24/7 glucose readings without needing to prick fingers.
2. Hyperglycemic Hyperosmolar State (HHS)
HHS is another acute complication of DM, typically occurring in older adults with type 2 diabetes. Unlike DKA, HHS doesn’t involve significant ketone production but leads to extremely high blood sugar levels. The body becomes severely dehydrated, leading to an electrolyte imbalance.
Symptoms:
- Very high blood sugar levels
- Dry mouth and skin
- Confusion or altered mental status
- Seizures (in severe cases)
Causes:
- Insulin deficiency, but less than in DKA
- Dehydration in diabetes
- Infections or other illnesses
Prevention:
- Adequate hydration
- Managing blood glucose fluctuations
- Regular blood glucose checks
3. Lactic Acidosis (LA)
Lactic acidosis is a rare but serious complication often associated with the use of certain medications, especially in people with kidney problems. In this condition, the body produces too much lactic acid, leading to metabolic acidosis.
Symptoms:
- Rapid breathing
- Abdominal discomfort
- Weakness
- Nausea and vomiting
- Altered mental status
Causes:
- Use of medications like metformin in people with poor kidney function
- Insulin deficiency
- Sepsis or severe infections
Prevention:
- Monitoring kidney function regularly
- Avoiding medications that can contribute to lactic acidosis in high-risk individuals
Did you know?
Taking insulin doses does not require injections anymore. Automatic insulin delivery (AID) systems like Omnipod 5 allow users take insulin doses with just a click. Check your eligibility with CGM Monitors today.
4. Hypoglycemia (Low Blood Sugar Emergency)
Hypoglycemia is one of the most common and severe hypoglycemia events that people with diabetes may face. This occurs when blood sugar levels drop too low, causing immediate symptoms that require fast action.
Symptoms:
- Shakiness
- Sweating
- Anxiety
- Altered mental status (confusion, irritability)
- Loss of consciousness in severe cases (insulin shock)
Causes:
- Too much insulin or medication
- Skipping meals
- Excessive exercise without adjusting insulin
- Drinking alcohol on an empty stomach
Prevention:
- Regular blood glucose monitoring
- Carrying quick sources of sugar (like glucose tablets or juice)
- Adjusting insulin doses to activity levels
Acute Complications of Diabetes: A Quick Overview
| Acute Complication | Probability | Possible Prevention Techniques |
| Diabetic Ketoacidosis (DKA) | High in type 1 diabetes; can occur in type 2 | Regular insulin management, infection control, and hydration |
| Hyperglycemic Hyperosmolar State (HHS) | Mostly in type 2 diabetes, particularly in older adults | Hydration, regular monitoring, and controlling blood sugar levels |
| Lactic Acidosis (LA) | Rare, but more likely with kidney problems | Kidney function monitoring, cautious use of certain medications |
| Hypoglycemia (Low Blood Sugar) | Common in insulin-treated individuals | Regular blood sugar checks, quick sugar sources, and meal planning |
A user expressed their constant worry about complications on Reddit, describing their experience on it: “I’ve developed extreme anxiety about developing some form of complications from diabetes… had full blown panic attack.” It shows the significant psychological impact and anxiety that the fear of diabetes complications can have on individuals, even when physical health is stable.
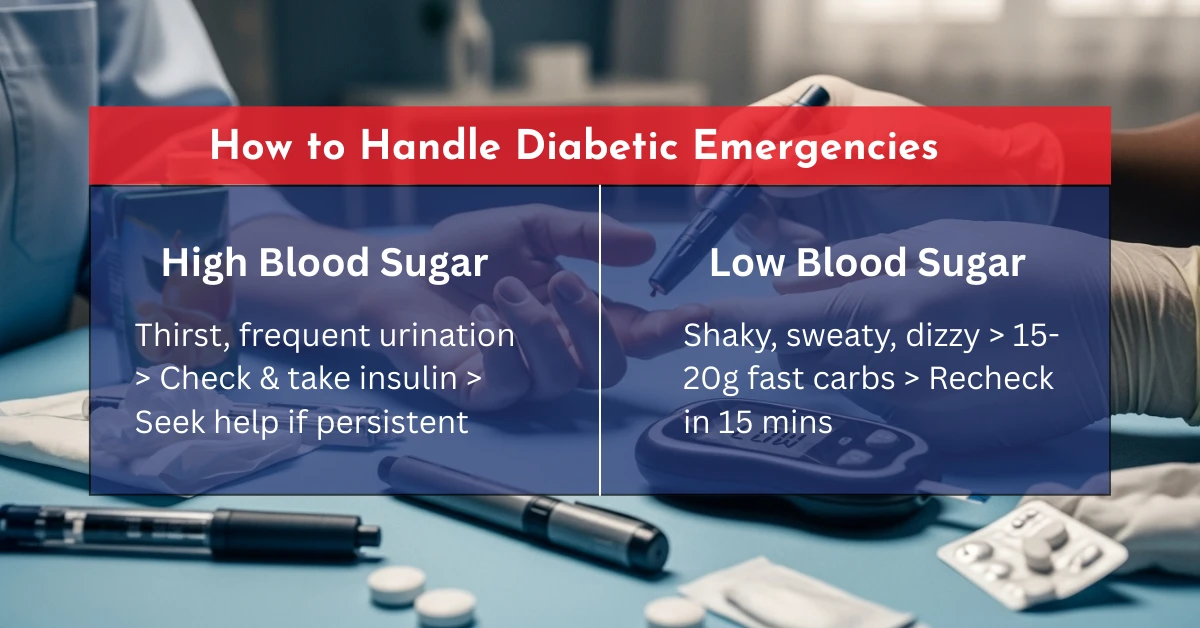
How to Handle Diabetic Emergencies
While you may be managing blood sugar properly, it’s important to recognize any emergency situations and take immediate first aid. However, people using CGM sensors are advised to first take a blood glucose test using a stick, especially if the glucose levels do not match the symptoms:
1. Dealing with Hyperglycemia (High Blood Sugar)
- Symptoms: Extreme thirst, frequent urination, dry mouth, blurry vision, and fatigue.
- Action: Check blood sugar levels and administer insulin if needed. If blood sugar remains high, seek emergency medical attention.
- Prevention: Ensure regular blood glucose monitoring and avoid long gaps without insulin or medication.
2. Managing Hypoglycemia (Low Blood Sugar)
- Symptoms: Shakiness, sweating, dizziness, confusion, rapid heart rate.
- Action: As suggested by the Mayo Clinic, consume 15-20 grams of fast-acting carbohydrates (e.g., glucose tablets or juice). Recheck blood sugar after 15 minutes. If still low, repeat.
- Prevention: Keep a glucose source handy, especially during physical activity. Adjust insulin doses when needed.
Conclusion
Whether you are dealing with hyperglycemia complications or facing a low blood sugar emergency, quick action is vital. As in case of hyperglycemia (high blood sugar), insulin is a life savior, any carb snack is in case of hypoglycemia (low blood sugar). On top of all these cures, remember that a healthy lifestyle with balanced diet, possible with controlled carbs, daily exercise, proper sleep, and stress management are all your best friends who can help you live a healthy life even in the presence of this health condition.
Consistent monitoring and proper management can help you keep blood glucose fluctuations under control while reducing the risks of an acute diabetic crisis.
Frequently Asked Questions
What is the acute emergency of diabetes?
Diabetic Ketoacidosis (DKA), Hyperglycemic Hyperosmolar State (HHS), Lactic Acidosis (LA), and Hypoglycemia (Low Blood Sugar Emergency) are all acute emergencies of diabetes. Causes, preventions, and cures can be found above.
What is the most common acute complication of type 1 diabetes?
Diabetic ketoacidosis (DKA), a life-threatening complication, is most common among type 1 diabetics. Happens when your body starts breaking fats for energy and your blood becomes acidic.
Which symptoms are associated with the acute complications of diabetes?
Symptoms can generally vary, such as in case of ketoacidosis, the person may experience vomiting, dehydration, fruity breath, and abdominal pain. While hypoglycemic event may show headache, irregular heartbeats, sweating, or shivering.
Can type 2 diabetics get DKA?
Yes, while the probability is higher in type 1 diabetics, people with type 2 diabetics may also experience it. Type 2 diabetics on keto diet should consult their doctors and use ketone strips for continuous monitoring of ketone bodies in their body.
Disclaimer: This blog is for informational purposes only and does not constitute medical, legal, or professional advice. While we strive for accuracy, errors or omissions may occur.



Write a comment
Your email address will not be published. All fields are required