Table of content
- The Biology Behind Pain-Induced Glucose Elevation:
- How Pain Affects the Body’s Stress Response
- Acute vs. Chronic Pain: Different Glucose Patterns
- Can Chronic Pain Raise Blood Sugar Over Weeks or Months?
- Why Does Pain Raise Blood Sugar?
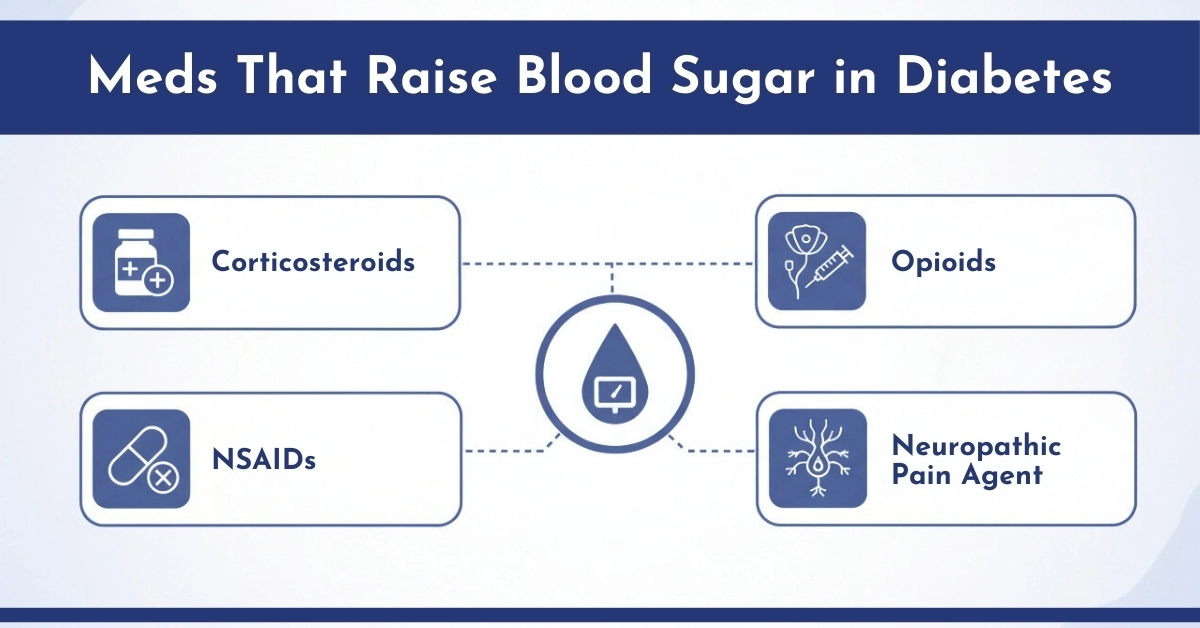
- Meds That Raise Blood Sugar in Diabetes
- Real Examples People With Diabetes Report
- How CGM Monitors Help Track Pain-Related Glucose Spikes
- What to Do When Pain Raises Your Blood Sugar
- Conclusion: Pain and Blood Sugar
- People Asked For
Can Pain Raise Blood Sugar? Indeed, the body’s response is something that can be measured and is of medical importance. Pain engages the body’s stress response system, which releases certain hormones that increase blood sugar levels even in the absence of food. This poses a problem for patients with diabetes, prediabetes, or those with metabolic syndrome: unexplained hyperglycemia during or following painful episodes.
Whether triggered by chronic pain, back pain, post-operative discomfort, or the use of certain analgesics, patients often experience elevated glucose levels—detected through Continuous Glucose Monitoring (CGM)—that are unrelated to food intake. Knowing this relationship helps in avoiding unwanted medication changes and provides better management of glucose control in real-time with CGM systems available at CGM Monitors.
The Biology Behind Pain-Induced Glucose Elevation:
While pain is discomforting to experience, it also activates the stress response of the body, which triggers the hypothalamic-pituitary-adrenal (HPA) axis, resulting in a cascade of hormonal changes. Some of these hormones are cortisol, epinephrine, and norepinephrine, which directly affect glucose metabolism.
Important Factors That Increase Glucose Levels During Pain:
- Cortisol: Causes greater insulin resistance and stimulates the release of glucose from the liver
- Epinephrine: Increases blood glucose concentration by inducing glycogenolysis
- Norepinephrine: Increases the vasoconstrictor effect on blood vessels and lowers insulin sensitivity
- Inflammatory cytokines (e.g., IL-6, TNF-α): Disrupt insulin pathways and β-cell function
This is why pain and stress raise blood sugar both directly (via hormones) and indirectly (via inflammation and poor insulin utilisation).
How Pain Affects the Body’s Stress Response
When your body experiences pain — whether from a sudden accident, inflammation, illness, or chronic discomfort- it always triggers a stress reaction. In response, the brain signals the adrenal glands to release stress hormones such as cortisol and adrenaline, as discussed above. These hormones are part of the “fight‑or‑flight” response and prepare your body to respond to danger by:
- Increasing glucose production in the liver
- Reducing insulin sensitivity
- Releasing stored energy into the bloodstream
This hormonal surge causes your blood sugar to rise temporarily because the body is mobilizing glucose as an energy source, even if you don’t actually need it at that moment. This response is similar to what happens with stress or emotional distress. (Source: Healthlines)
Acute vs. Chronic Pain: Different Glucose Patterns
The duration and intensity of pain affect how blood glucose behaves. CGM data shows distinct trends in acute vs. chronic pain states.
Acute Pain (Short‑Term)
No need of worry situation because it is a short bursts of pain — like from a minor injury or surgery — can lead to a temporary glucose spike. The body releases stress hormones quickly to cope with the pain, which can cause blood sugar to rise for several hours. Once the pain and stress response subside, levels often trend back toward normal.
Chronic Pain (Long‑Term)
Persistent, ongoing pain — such as from arthritis, neuropathy, or chronic inflammation — can create a sustained elevation in stress hormones. This continuous stress signal makes insulin less effective (known as insulin resistance) and can contribute to consistently higher blood glucose readings over time.
| Pain Type | Duration | Glucose Pattern Seen in CGM |
| Acute Pain | Minutes to Hours | Sudden glucose spike, resolves as pain subsides |
| Chronic Pain | Weeks to Years | Persistent mild elevations, higher morning fasting levels |
| Severe Pain | Ongoing, Intense | Sustained elevations, often 20–40 mg/dL above baseline |
Can Chronic Pain Raise Blood Sugar Over Weeks or Months?
Absolutely. Chronic pain contributes to sustained hormonal stress, which worsens insulin sensitivity over time. This elevates fasting glucose levels, particularly in the morning (also known as the dawn phenomenon). Pain conditions strongly linked with chronic hyperglycemia include:
- Sciatica
- Diabetic neuropathy
- Osteoarthritis
- Post-surgical pain
- Rheumatoid arthritis
Patients often need therapy adjustments during periods of high pain to stabilize glucose.
Back Pain and Diabetes
Back pain is associated with inflammation, reduced mobility, and disrupted sleep—all of which contribute to hyperglycemia. Those with lumbar disc disease or muscle spasms often report elevated fasting blood glucose, especially on CGM. Even non-diabetic patients may experience glucose intolerance when back pain becomes chronic.
Why Does Pain Raise Blood Sugar?
Here’s what happens inside the body:
1. Stress Hormones Increase Glucose Production
Cortisol and adrenaline stimulate the liver to release more glucose into the bloodstream. This was an evolutionary survival response, but in people with diabetes, it can cause unwanted spikes.
2. Insulin Sensitivity Decreases
When stress hormones are high, the body’s cells become less responsive to insulin — a condition known as insulin resistance. This means the same amount of insulin does less to lower blood glucose.
3. Inflammation Makes Control Harder
Chronic pain often comes with inflammation, which itself can interfere with glucose regulation and insulin action.
4. Lifestyle Factors Compound the Effect
Pain can limit physical activity, disrupt sleep, and even cause emotional stress — all of which can further destabilize blood sugar levels.
Meds That Raise Blood Sugar in Diabetes
Certain medications prescribed to manage pain can elevate blood glucose levels both directly and indirectly. With that in mind, here’s some key information:
Corticosteroids (Prednisone, methylprednisolone):
These drugs literally and figuratively ‘bring sugar’ as they raise blood sugar levels by increasing glucose production in the liver and worsening insulin resistance.
Opioids (Morphine, Oxycodone):
May blunt insulin secretion and cause erratic appetite leading to worsening blood sugar levels.
NSAIDs (Naproxen, Ibuprofen):
While mostly safe as far as glucose control is concerned, their use could lead to chronic kidney disease which is known to worsen diabetes control.
Neuropathic pain agents (e.g., gabapentin, pregabalin):
Associated with weight gain and glucose imbalance during extended use.
Real Examples People With Diabetes Report
Many people with diabetes share personal experiences on Reddit that show this effect: long periods of pain often coincide with higher glucose readings, even without eating more or changing medications. This supports the idea that pain‑induced stress responses can really affect glucose levels in day‑to‑day life. (Source: r/type1diabetes)
Pain=Stress and results is an increase in Sugar levels.
How CGM Monitors Help Track Pain-Related Glucose Spikes
Traditional glucose meters only offer single-point readings. In contrast, CGM monitors track your glucose patterns 24/7, showing how pain, stress, or medication changes affect your body.
With CGM technology, users can:
- Identify unexplained glucose elevations
- Correlate pain episodes to specific glucose trends
- Fine-tune insulin or oral medications
- Detect overnight hyperglycemia linked to pain-induced sleep disruptions
Start with clinically approved CGMs from CGM Monitors, designed for both patient and provider decision-making.
What to Do When Pain Raises Your Blood Sugar
- Use a CGM Monitor’s Products: This is essential for pattern tracking.
- Document pain intensity: Use a daily log to compare against CGM readings.
- Review medications: Ask your provider which pain meds raise blood sugar and request alternatives.
- Focus on sleep: Poor sleep worsens pain and insulin resistance—prioritize core sleep to support glucose control and recovery.
- Prioritize Anti-inflammatory foods: Omega-3s, green vegetables, turmeric, or protein shakes may help lower inflammation and glucose.

Conclusion: Pain and Blood Sugar
Pain doesn’t just hurt—it elevates blood sugar through hormonal and inflammatory pathways.
If you’ve ever asked, does pain increase blood sugar levels? It is a yes, but for many patients, this is more common than we believe. These spikes can be tracked in real time with CGM monitors which can help devise better treatment plans for sustained glucose control. Visit CGM Monitors to explore clinically tested CGM systems designed for real-world conditions like pain-induced hyperglycemia.
People Asked For
How does acute pain affect blood glucose readings in non-diabetics?
Acute pain triggers stress hormones like cortisol and adrenaline, causing short-term insulin resistance and increased liver glucose production, which can temporarily raise blood sugar even in non-diabetics. Severe pain or procedures can cause larger spikes.
How can I manage pain to prevent blood sugar spikes?
Maintain steady blood sugar with low-impact exercises like yoga or swimming, a high-fiber diet, and mind-body practices. Consult your doctor about safe pain relievers and supplements to reduce stress-induced spikes.
How do pain medications affect blood sugar levels?
Pain medications vary in effect: opioids may lower or raise glucose, corticosteroids can increase it, and NSAIDs may slightly reduce it. Always monitor your blood sugar and follow clinician guidance when changing medications.
What is the connection between pain and elevated blood sugar levels?
Pain triggers stress hormones that increase liver glucose production and impair insulin action. Chronic pain and inflammation can worsen this effect, making pain management critical for blood sugar stability.
Who is most at risk for blood sugar spikes due to pain?
Diabetics, prediabetics, chronic pain sufferers, obese individuals, and those with poor self-management habits are most at risk. Acute severe pain may also temporarily raise glucose in non-diabetics.
When should I be concerned about pain-induced blood sugar increases?
Seek medical advice if blood sugar consistently exceeds 180 mg/dL during pain, especially with symptoms like frequent urination, thirst, or fatigue, as it may indicate worsening insulin resistance.
When does pain-related hyperglycemia become a medical emergency?
Hyperglycemia above 250-300 mg/dL with ketones, nausea, vomiting, or confusion is an emergency. Immediate ER care is required to prevent diabetic ketoacidosis or organ damage.
Why does chronic pain seem to have a different impact on blood sugar than acute pain?
Chronic pain causes persistent stress and inflammation, leading to sustained blood sugar increases and reduced self-management. Acute pain produces short-term spikes that subside once pain decreases.
Why does pain cause blood sugar to rise, especially in individuals with diabetes?
Pain intensifies stress hormones that block insulin action, increase liver glucose, and reduce cellular glucose uptake, making diabetics more vulnerable to significant spikes and complications like neuropathy.
Why is it important for diabetics to monitor blood sugar during painful episodes?
Monitoring allows early detection and management of spikes, adjustment of insulin or lifestyle, and reduces the risk of complications, promoting better long-term health.




Write a comment
Your email address will not be published. All fields are required