Table of content
- Can Type 2 Diabetes Turn Into Type 1 Diabetes?
- Symptoms Indicating a Shift Toward Autoimmune Diabetes
- Factors That Mimic a Shift from Type 2 to Type 1 Diabetes
- Medical Interventions and Management Strategies
- Diagnostic Methods for Identifying Type 1 vs. Type 2 Diabetes
- Comprehensive Comparison Table: Type 1 vs. Type 2 Diabetes
- Final Words
- Frequently Asked Questions
More than 37 million people across the US have diabetes. About 90% have type 2 diabetes, while 5-10% have type 1. Both types of diabetes affect the insulin-related regulation of glucose, but they differ in their causes and duration of onset, and treatment. A few patients inquire can type 2 diabetes turn to Type 1 Diabetes; however, these are two distinct conditions that have no clear progression from one to the other.
But misdiagnosis and similar features, especially for adults, could confuse the diabetic. Understanding these differences is crucial. This article reviews the facts about Type 1 and Type 2 diabetes and explores conditions that Type 2 diabetic patients should consider to determine whether their condition may be progressing toward Type 1 diabetes.
Can Type 2 Diabetes Turn Into Type 1 Diabetes?
From a medical point of view, Type 2 diabetes does not transform into Type 1 diabetes, as they are separate conditions with different underlying causes. However, there is a condition known as Latent Autoimmune Diabetes in Adults (LADA), often referred to as “Type 1.5 diabetes,” which exhibits features of both types, and that is the only reason to raise such a question in the diabetic person.
LADA typically starts with insulin resistance like Type 2 diabetes but gradually progresses to autoimmune destruction of beta cells, a hallmark of Type 1 diabetes. This explains why some adults initially diagnosed with Type 2 diabetes may eventually require insulin therapy similar to Type 1 management.
Key Insight For You: Although Type 2 diabetes itself cannot become Type 1, certain autoimmune processes can develop over time, making insulin therapy essential for optimal blood sugar control.
Symptoms Indicating a Shift Toward Autoimmune Diabetes
Recognizing early warning signs can help manage the progression of diabetes effectively. Patients with Type 2 diabetes who notice these symptoms should consult their healthcare provider immediately:
- Rapid weight loss without trying
- Frequent urination and excessive thirst
- Fatigue and general weakness
- Increased blood sugar levels despite lifestyle management
- Signs of autoimmune activity such as skin rashes or thyroid issues
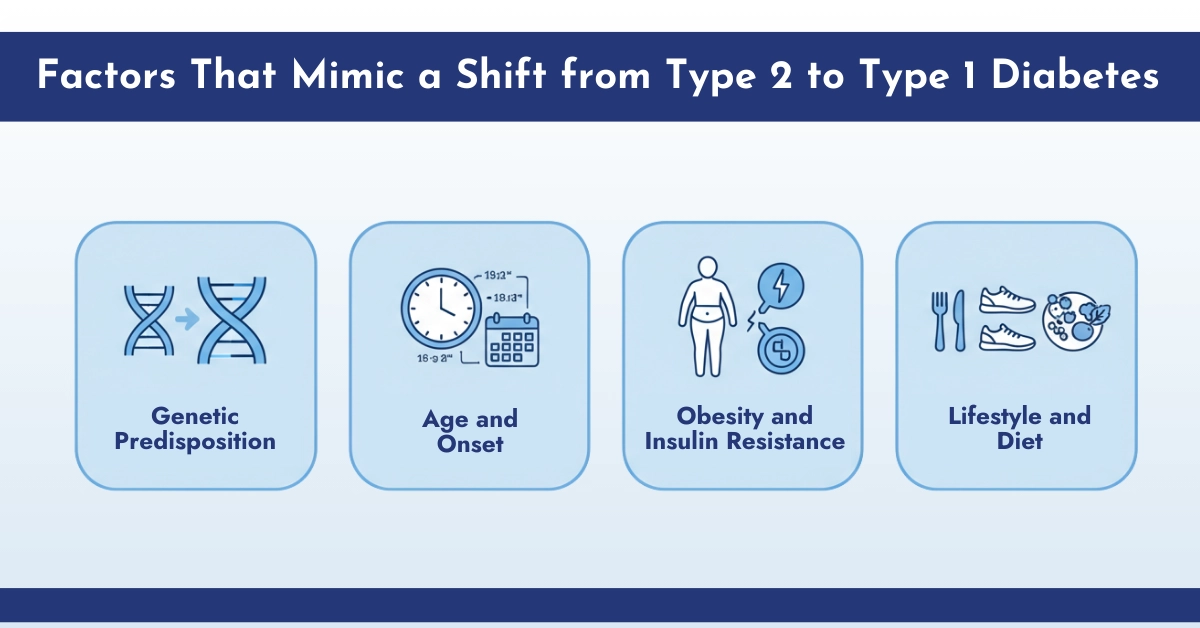
Factors That Mimic a Shift from Type 2 to Type 1 Diabetes
Certain factors can accelerate beta-cell dysfunction, making Type 2 diabetes appear similar to Type 1:
- Genetic Predisposition: Family history of Type 1 diabetes increases the likelihood of autoimmune involvement.
- Age and Onset: Adults diagnosed with Type 2 at a younger age may experience faster beta-cell deterioration.
- Obesity and Insulin Resistance: Prolonged insulin resistance can stress beta cells, sometimes triggering autoimmune responses.
- Lifestyle and Diet: High-sugar diets, lack of exercise, and chronic stress contribute to accelerated pancreatic dysfunction.
Medical Interventions and Management Strategies
Patients concerned about the potential progression of diabetes can benefit from a structured management plan. Here’s what healthcare professionals recommend:
1. Early Diagnosis and Monitoring
Routine blood tests, including fasting glucose, A1C, C-peptide, and autoantibody screening, are critical. These tests help identify whether insulin therapy might become necessary and provide early detection of autoimmune involvement.
2. Lifestyle Modifications
- Balanced Diet: Incorporate high-fiber foods, lean protein such as lentils, and low-glycemic carbohydrates to stabilize blood sugar.
- Regular Exercise: Strength training and aerobic activity improve insulin sensitivity.
- Weight Management: Maintaining a healthy weight reduces the risk of beta-cell stress.
3. Medications and Insulin Therapy
While most Type 2 diabetes patients start with oral medications like metformin, some may eventually require insulin if beta-cell function declines. In cases of LADA or autoimmune involvement, early initiation of insulin can preserve residual beta-cell activity and improve long-term outcomes.
4. Continuous Glucose Monitoring (CGM)
Advanced CGM devices like the new Dexcom G7 sensor and Libre 3 Plus, provide real-time insights into glucose patterns, helping both patients and doctors make precise adjustments to medications, diet, and lifestyle.
Diagnostic Methods for Identifying Type 1 vs. Type 2 Diabetes
- Autoantibody testing: Over 90% of people with type 1 diabetes have antibodies targeting pancreatic beta cells. Their presence strongly supports a diagnosis of type 1.
- C-peptide levels: The test shows the amount of insulin your body creates. Low levels are common in type 1, but they also appear in longstanding type 2 cases with advanced pancreatic decline.
- Clinical presentation and age: Adult cases of Type 1 diabetes do happen. Similarly, type 2 is now being identified in younger individuals, especially in those with elevated BMI. Age alone is not a reliable diagnostic marker.

Comprehensive Comparison Table: Type 1 vs. Type 2 Diabetes
| Feature | Type 1 Diabetes | Type 2 Diabetes |
| What happens in the body? | The immune system destroys insulin-producing cells | The body stops responding well to insulin; production drops over time |
| Insulin production | None or nearly none | Starts off normal, then decreases |
| Need for insulin | Always required from the start | Might be needed later, depending on progression |
| How fast does it appear? | Sudden, especially in younger people | Develops slowly—often goes unnoticed |
| Who gets it? | Often diagnosed in kids or teens, but it can happen at any age | Common in adults, now rising in teens and children, too |
| Symptoms | Quick onset: weight loss, thirst, frequent urination, fatigue | Slow onset: tiredness, blurry vision, slow healing, more urination |
| Weight at diagnosis | Usually lean or normal weight | Often above the recommended weight range |
| Family history | Linked to autoimmune conditions like thyroid or celiac disease | More often runs in families with type 2 or pregnancy-related diabetes |
| How it’s diagnosed | Blood sugar, antibody tests, and C-peptide levels | Blood sugar and C-peptide antibody tests are usually negative |
| Role of lifestyle | Helps control, but doesn’t prevent or stop the condition | Key to delaying, managing, or even improving the condition |
| Can it be reversed? | No | Some cases can improve significantly with long-term changes |
| Ongoing care | Daily insulin, CGM, meal planning, endocrinologist support | Diet, activity, medication, glucose monitoring, and regular doctor visits |
| Ketoacidosis risk | High if insulin is missed | Rare, but it can happen in later stages |
Final Words
Type 1 and type 2 diabetes are distinct. Type 1 diabetes is caused by autoimmune insulin insufficiency, whereas type 2 diabetes is caused by increasing insulin resistance. Although one does not develop into the other, both eventually need insulin, underscoring the significance of a precise diagnosis and individualised care. Both diseases carry risk for neurologic, vascular, and renal problems if they are not properly addressed. So, it is important to manage insulin-dependent Type 2 or 1 diabetes diagnosis by individualised care using CGMs to avoid the risk of complications.
Frequently Asked Questions
How does Type 2 diabetes differ from Type 1 diabetes in terms of insulin production?
In Type 1 diabetes, the immune system destroys pancreatic beta cells, leading to little or no insulin production, requiring lifelong insulin therapy. In Type 2 diabetes, the body produces insulin but develops resistance, with beta cells initially overproducing insulin before gradually failing, often manageable initially with lifestyle changes and oral medications.
What is LADA and how is it related to Type 2 diabetes progression?
LADA (Latent Autoimmune Diabetes in Adults), also called Type 1.5 diabetes, is a slow-progressing autoimmune form of Type 1 diabetes that appears in adulthood. It is often misdiagnosed as Type 2 due to similar presentation but involves gradual beta-cell destruction like Type 1, eventually requiring insulin as oral treatments fail.
How can doctors differentiate between Type 2 diabetes evolving and LADA?
Doctors differentiate by testing for autoimmune antibodies (e.g., GAD, IA-2), which are positive in LADA but absent in classic Type 2. Additional clues include lower BMI, lack of metabolic syndrome features, lower C-peptide levels, and poor response to oral medications.
Why might someone with Type 2 diabetes eventually require insulin like a Type 1 diabetic?
Progressive beta-cell exhaustion from chronic insulin resistance reduces insulin production over time. As the pancreas can no longer compensate, blood glucose control worsens, necessitating exogenous insulin supplementation, though some residual production often remains.
Can Type 2 diabetes truly turn into Type 1 diabetes?
No, Type 2 diabetes cannot turn into Type 1, as they have distinct causes. However, some adults initially diagnosed with Type 2 actually have LADA (slow-onset autoimmune diabetes), which progresses to insulin dependence.
When should a Type 2 diabetic be tested for autoimmune markers?
Testing for antibodies (e.g., GAD) is recommended if diagnosed as Type 2 but with atypical features: adult onset yet lean BMI, no family history of Type 2, poor response to oral meds, or coexisting autoimmune conditions. Rapid deterioration despite treatment is also a signal for testing.
Why are the treatment approaches for Type 1 and Type 2 diabetes so distinct?
Type 1 requires immediate lifelong insulin replacement since no endogenous insulin is produced. Type 2 initially targets insulin resistance with lifestyle changes, oral agents, or injectables, adding insulin later if beta cells fail.
What factors contribute to beta cell dysfunction in Type 2 diabetes?
Key factors include chronic hyperglycemia (glucotoxicity) and elevated free fatty acids (lipotoxicity), causing oxidative stress, inflammation, and ER stress. Obesity-driven insulin resistance increases beta-cell demand, leading to exhaustion, apoptosis, and dedifferentiation over time.
Is diabetes genetic, type 1 or type 2?
Both forms have genetic links. Type 2 diabetes has a stronger hereditary pattern, often running in families.
Which is worse: type 1 diabetes or type 2 diabetes?
Type 1 diabetes is considered more severe due to complete insulin deficiency and its autoimmune origin. Still, both types carry long-term risks and require precise glucose control.
Can type 2 diabetes be reversed or cured?
Type 2 diabetes has no cure, but it can enter remission through weight loss, diet, and physical activity.
Can adults develop type 1 diabetes?
Yes. Though often diagnosed in youth, type 1 diabetes can appear at any age due to autoimmune pancreatic damage.
How is LADA different from type 2 diabetes?
LADA shares features of both types. Unlike type 2 diabetes, insulin eventually becomes necessary.
Do type 1 and type 2 diabetes have different risk factors?
Yes. Type 1 involves autoimmune triggers and genetic predisposition. Type 2 is influenced by age, ethnicity, weight, and lifestyle, but can be delayed through lifestyle changes.
Can someone have both type 1 and type 2 diabetes?
Yes. People with type 1 sometimes develop insulin resistance, leading to “double diabetes.”



Write a comment
Your email address will not be published. All fields are required