Table of content
Dry mouth, also known as xerostomia, is a common issue for many people with diabetes. If you’ve been experiencing an unusual level of dryness in your mouth, it’s important to understand how diabetes might be contributing to this problem and what you can do to manage it. In this blog, we’ll explore the connection between diabetes and dry mouth, its causes, and practical solutions to help you find relief.
What is Dry Mouth: Xerostomia?
Dry mouth, or xerostomia, is the sensation of having insufficient saliva in the mouth. In diabetes, it can manifest as:
- Diabetic cotton mouth
- Dry lips diabetes
- Sticky lips diabetes
- Dry throat diabetes
Unlike occasional mouth dryness from dehydration or environmental factors, diabetes-related dry mouth is chronic and persistent, often interfering with eating, speaking, and swallowing. People with diabetes dry lips may notice discomfort, especially in the morning or at night, signalling the need for better blood sugar and oral management.
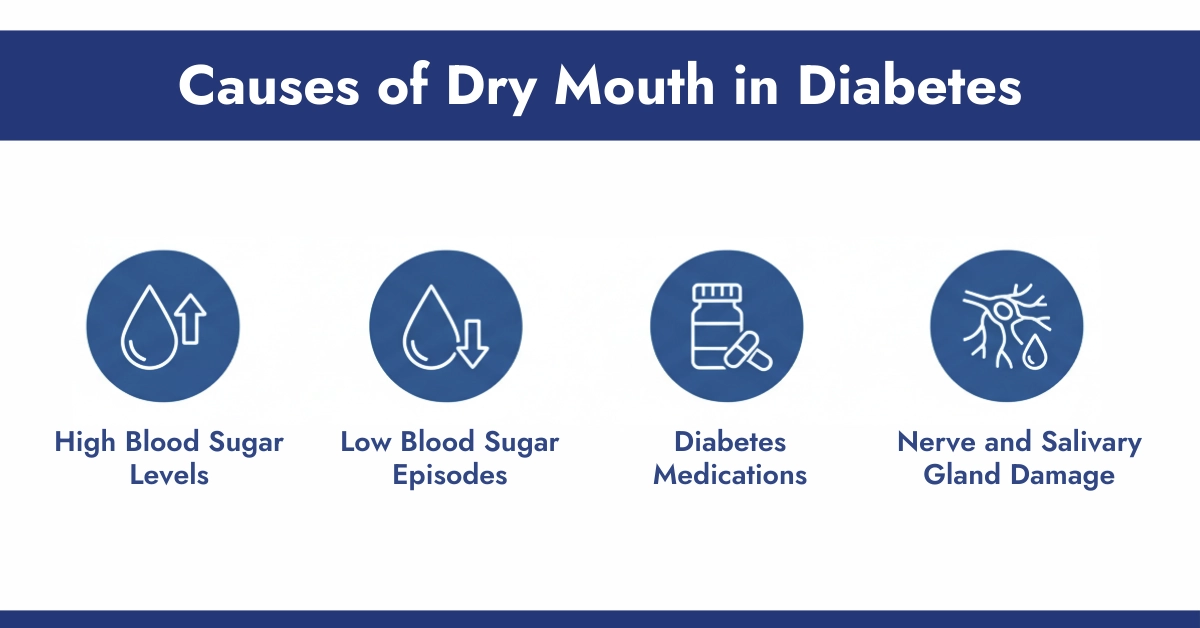
Causes of Dry Mouth in Diabetes
Several factors contribute to dry mouth diabetes, ranging from blood sugar imbalances to medication side effects.
a. High Blood Sugar Levels
Hyperglycemia, or high blood sugar, causes your body to lose fluids, leading to dehydration. This directly affects saliva production, causing dry mouth blood sugar issues. People with uncontrolled diabetes may often feel thirsty and notice persistent mouth dryness.
b. Low Blood Sugar Episodes
Interestingly, low blood sugar (hypoglycemia) can also trigger dry mouth. During hypoglycemia, the body responds with stress hormones that reduce saliva flow. People may wonder, can low blood sugar cause dry mouth? Yes, especially if blood sugar swings are frequent.
c. Diabetes Medications
Certain medications used to manage diabetes can cause xerostomia. For instance:
- Metformin dry mouth: Commonly reported by users, sometimes worse at night
- Insulin: Rarely, insulin therapy may contribute indirectly to dry mouth
- Other diabetes medications may reduce saliva production or alter oral pH
d. Nerve and Salivary Gland Damage
Long-term diabetes can lead to neuropathy, affecting the nerves that control salivary glands. Damage to these nerves results in chronic diabetes xerostomia, where the mouth feels dry regardless of fluid intake.
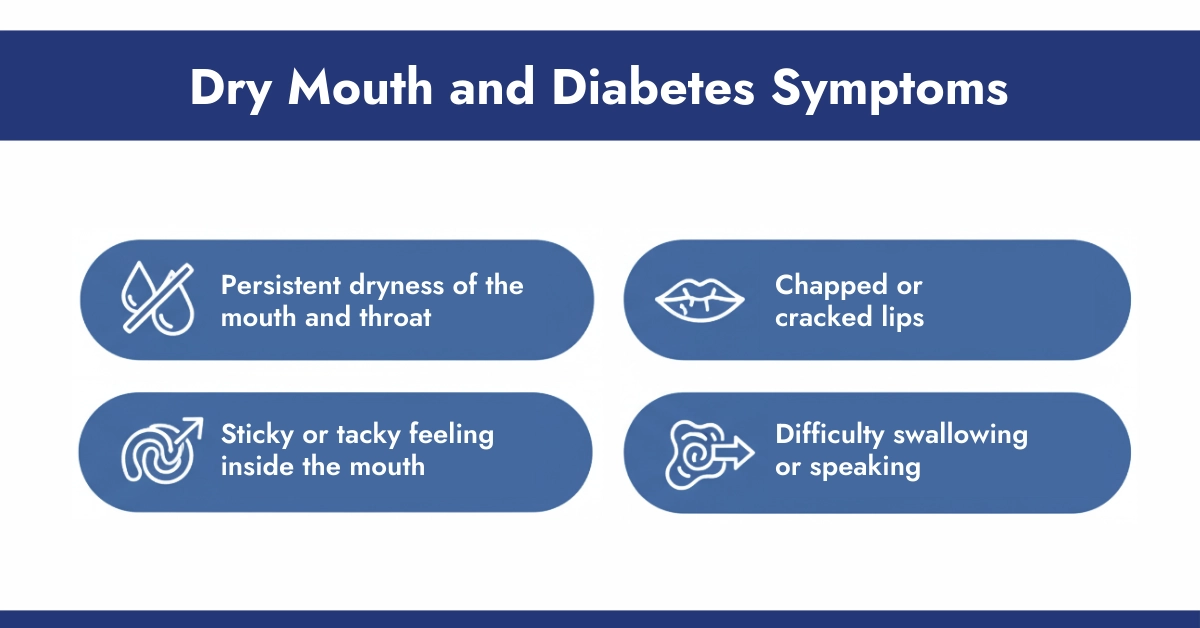
Dry Mouth and Diabetes Symptoms
Dry mouth, also known as xerostomia, is a common symptom in people with diabetes. Recognizing it early can help manage discomfort and prevent complications. Key signs include:
1. Persistent dryness of the mouth and throat
People with diabetes may feel constant dryness in their mouth or throat, even after drinking water. This can make talking, eating, and swallowing uncomfortable.
2. Chapped or cracked lip
Reduced saliva can lead to dry, chapped, or cracked lips. This symptom may worsen in cold or dry weather and can cause soreness or bleeding if left untreated.
3. Sticky or tacky feeling inside the mouth
A sticky or tacky sensation on the tongue or roof of the mouth is often noticeable in diabetes-related dry mouth. It can make it difficult to taste food properly and affect oral hygiene.
4. Difficulty swallowing or speaking
Severe dryness can interfere with normal speech or swallowing. People may find it harder to chew or swallow certain foods and may notice their voice becoming hoarse.
Understanding these symptoms is important for distinguishing between occasional dryness and xerostomia caused by diabetes. Managing blood sugar levels, staying hydrated, and using saliva substitutes can help alleviate discomfort and protect oral health.
Health Risks of Untreated Dry Mouth
Neglecting dry mouth in diabetics can lead to serious oral health issues:
- Cavities and tooth decay: Saliva protects teeth; lack of it increases risk
- Gum disease (gingivitis or periodontitis)
- Oral infections: Fungal infections like thrush are common
- Impact on blood sugar control: Difficulty eating due to dry mouth can affect nutrition and glucose management
Remedies and Treatments for Diabetes Dry Mouth in Diabetes
a. Lifestyle & Home Remedies
Simple adjustments can reduce diabetes dry mouth symptoms:
- Stay hydrated: Drink water regularly
- Check blood sugar regularly: Use Dexcom G7 or Libre 3 Plus to monitor your sugar level every 5 minutes.
- Reduce sugar intake: Excess sugar worsens dehydration and oral bacteria growth
- Avoid alcohol and caffeine: Both can dehydrate the body
- Use sugar-free gum or lozenges: Stimulates saliva production
- Maintain good oral hygiene with gentle brushing
b. Medical Treatments
For persistent xerostomia diabetes, medical options include:
- Prescription saliva substitutes or oral moisturizers
- Adjusting diabetes medications under a doctor’s supervision to reduce side effects
- Regular dental check-ups to manage oral complications
When to Seek Professional Help
If diabetes and dry mouth persists despite trying these measures, or if it leads to severe discomfort or complications, it’s important to consult with your healthcare provider or dentist. They can help determine the underlying cause and recommend appropriate treatments or adjustments to your diabetes management plan.
Conclusion
The connection between diabetes and dry mouth is strong and often overlooked. Persistent xerostomia can lead to oral health problems, discomfort, and even affect blood sugar control. Proactive management through hydration, oral care, lifestyle changes, and regular medical consultations can significantly improve quality of life for people with diabetes. Understanding your symptoms and acting early is the key to preventing long-term complications.
References:
- Cleveland Clinic: Diabetes and Dry Mouth
- Healthline: Dry Mouth Diabetes
Frequently Asked Questions
How does diabetes cause dry mouth?
Diabetes often leads to dry mouth because high blood sugar levels can reduce saliva production in the salivary glands, leading to dehydration and impaired moisture in the mouth. This condition, known as xerostomia, is exacerbated by frequent urination that depletes body fluids, making the oral environment feel parched and uncomfortable for many patients.
How can diabetics alleviate dry mouth symptoms effectively?
Diabetics can alleviate dry mouth by staying well-hydrated with frequent sips of water, using sugar-free lozenges or gum to stimulate saliva flow, and avoiding caffeine or alcohol which can worsen dehydration. Maintaining good blood sugar control through diet and using CGM sensors listed on CGM Monitors also helps reduce the severity of symptoms over time.
What is the connection between diabetes and dry mouth?
The connection between diabetes and dry mouth stems from elevated glucose levels that disrupt saliva production and cause overall dehydration due to increased urination. This results in a drier oral cavity, increasing the risk of related issues like infections, and it’s a common indicator of uncontrolled blood sugar in diabetic individuals.
What are the early signs of dry mouth in diabetics?
Early signs of dry mouth in diabetics include a persistent sticky or dry feeling in the mouth, difficulty swallowing or speaking, and a burning sensation on the tongue. Patients may also notice cracked lips, increased thirst, or a change in taste, signaling the need to monitor blood sugar levels closely.
What are the best over-the-counter remedies for diabetic dry mouth?
The best over-the-counter remedies for diabetic dry mouth include saliva substitutes like mouth sprays or gels that provide moisture without sugar, and biotin-based mouthwashes designed for dry mouth relief. Sugar-free lozenges or xylitol gum can also stimulate natural saliva production while being safe for blood sugar management.
Why is dry mouth a common symptom for people with diabetes?
Dry mouth is a common symptom for people with diabetes due to hyperglycemia reducing saliva flow and causing dehydration from excessive urine output. This imbalance affects the mouth’s natural lubrication, making it a frequent complaint that highlights the importance of consistent glucose monitoring.
Why is managing dry mouth important for overall diabetic health?
Managing dry mouth is important for overall diabetic health because it prevents complications like tooth decay, gum disease, and oral infections that can worsen with reduced saliva. Proper management supports better oral hygiene, reduces discomfort, and helps maintain stable blood sugar levels to avoid further health issues.
Which type of diabetes is more commonly associated with dry mouth?
Type 2 diabetes is more commonly associated with dry mouth, as it often involves insulin resistance leading to prolonged high blood sugar levels that impair saliva production. However, both type 1 and type 2 can cause this symptom, though it’s frequently reported in unmanaged type 2 cases.
How to relieve dry mouth from diabetes?
To relieve dry mouth from diabetes, focus on hydration by drinking water regularly, using humidifiers to add moisture to the air, and chewing sugar-free gum to encourage saliva. Combining this with tight blood sugar control through lifestyle adjustments can provide long-term relief and minimize recurrence.











Write a comment
Your email address will not be published. All fields are required