Table of content
- Understanding Gluten: What You Need to Know
- Does Gluten Directly Affect Blood Sugar Levels?
- The Connection Between Gluten and Type 1 Diabetes
- Gluten and Type 2 Diabetes: What’s the Link?
- Should You Follow a Gluten-Free Diet for Diabetes?
- Potential Benefits of Going Gluten-Free
- Smart Carbohydrate Choices for Diabetes Management
- Practical Tips for Managing Gluten and Blood Sugar
- Conclusion
Living with diabetes (Typ2 and type 1) means making informed food choices every single day. If you’ve been wondering whether gluten affects your blood sugar levels or if going gluten-free could help manage your diabetes, you’re not alone. This comprehensive guide explores the relationship between gluten and diabetes, helping you make confident dietary decisions.
Key Takeaways:
- Gluten doesn’t directly raise blood sugar, but meals with carbohydrates and a glycemic index do.
- People with type 1 diabetes should be screened for celiac disease.
- A gluten-free diet isn’t automatically healthier unless medically necessary.
- Focus on whole, minimally processed foods regardless of gluten content.
- Individual testing and monitoring are essential for personalized management.
Understanding Gluten: What You Need to Know
Gluten is a protein naturally found in wheat, barley, and rye. It’s what gives bread its chewy texture and helps pasta hold its shape. While most people digest gluten without any problems, some individuals experience adverse reactions that can complicate diabetes management. For people living with diabetes, the connection between gluten and blood sugar control isn’t always straightforward. Let’s break down what really matters.
Does Gluten Directly Affect Blood Sugar Levels?
Here’s the truth for diabetic patients: gluten itself doesn’t raise blood sugar. What matters is the type of food containing gluten and its overall carbohydrate content. Many gluten-containing foods like white bread, pastries, crackers, and regular pasta are made from refined flour. These foods have a high glycemic index, meaning they cause rapid spikes in blood glucose. However, it’s the refined carbohydrates, not the gluten protein, that affect your blood sugar.
Think of it this way for your ease: a slice of whole wheat bread and a sugary doughnut both contain gluten, but they impact your body very differently. The whole wheat bread has more fiber and nutrients, leading to a slower, more stable rise in blood sugar. The donut, loaded with refined flour and sugar, causes a sharp glucose spike
It is recommended to use lentils because they have a low glycemic value and are the best of all among the diabetic friendly meals for diabetics.
The Connection Between Gluten and Type 1 Diabetes
If you have type 1 diabetes, understanding gluten becomes particularly important. Research shows that people with type 1 diabetes have a higher risk of developing celiac disease, an autoimmune condition where consuming gluten triggers an immune response that damages the small intestine.
Why This Matters
The overlap between type 1 diabetes and celiac disease isn’t coincidental. Both are autoimmune conditions with shared genetic factors. Studies indicate that approximately 4-9% of people with type 1 diabetes also have celiac disease, compared to just 1% of the general population.
If you have both conditions, undiagnosed celiac disease can create serious complications:
- Impaired nutrient absorption, making it harder to stabilise blood sugar
- Unpredictable blood glucose levels due to malabsorption
- Vitamin and mineral deficiencies that affect overall health
- Increased inflammation throughout the body
If you experience unexplained digestive issues, persistent fatigue, or difficulty maintaining stable blood sugar despite careful management, ask your healthcare provider about celiac disease screening.
Gluten and Type 2 Diabetes: What’s the Link?
For people with type 2 diabetes, gluten typically isn’t a direct concern unless you also have celiac disease or gluten sensitivity. The primary focus should be on managing insulin resistance and overall carbohydrate intake.
However, many processed gluten-containing foods contribute to challenges in type 2 diabetes management:
- Weight gain from calorie-dense refined grain products
- Blood sugar spikes from high glycemic index foods
- Increased inflammation from ultra-processed foods
- Poor nutrient density in refined grain products
The solution isn’t necessarily removing gluten—it’s choosing higher-quality carbohydrates and managing portion sizes.
Should You Follow a Gluten-Free Diet for Diabetes?
A gluten-free diet isn’t automatically better for blood sugar control. In fact, many gluten-free products are highly processed and contain more sugar, fat, and calories than their gluten-containing counterparts.
When a Gluten-Free Diet Makes Sense
You should follow a strict gluten-free diet if you have:
- Diagnosed celiac disease (absolutely essential).
- Non-celiac gluten sensitivity with confirmed symptoms.
- Type 1 diabetes with unexplained symptoms that might indicate undiagnosed celiac disease.
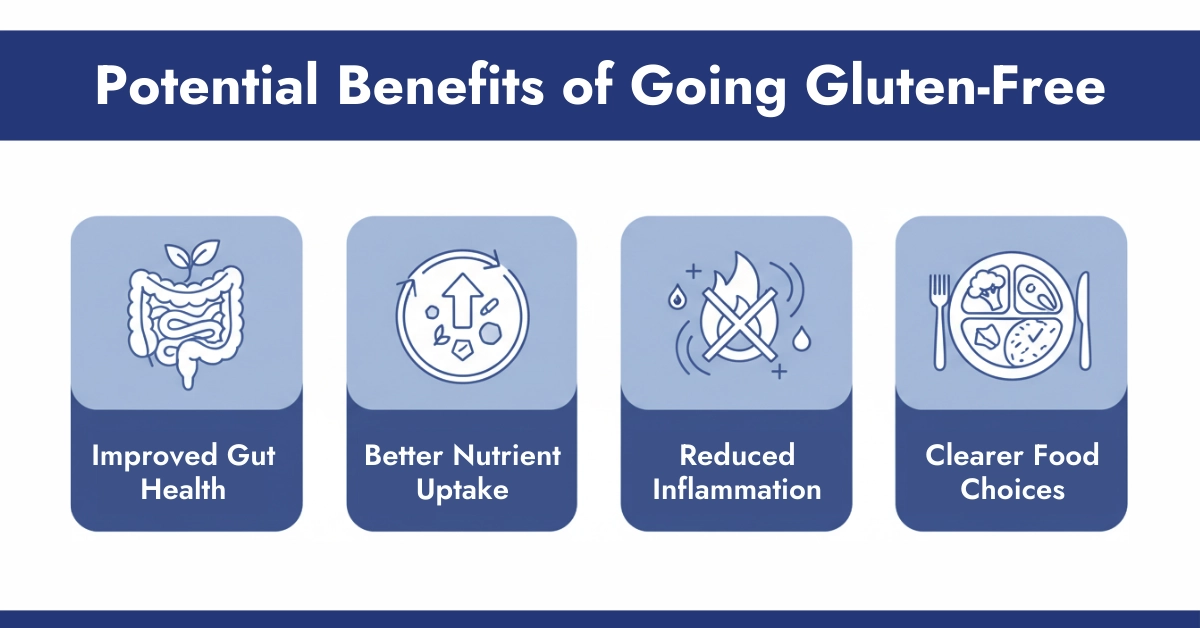
Potential Benefits of Going Gluten-Free
For those who truly need it, a gluten-free diet can offer:
- Improved Gut Health: Reducing intestinal inflammation allows better nutrient absorption, which can stabilize blood sugar patterns.
- Better Nutrient Uptake: When your gut heals, you absorb vitamins and minerals more efficiently, supporting overall diabetes management.
- Reduced Inflammation: Less systemic inflammation can improve insulin sensitivity in some individuals.
- Clearer Food Choices: Eliminating gluten often means cutting out processed foods, naturally leading to healthier eating patterns.
Smart Carbohydrate Choices for Diabetes Management
Whether you choose to eat gluten or not, focusing on smart carbohydrate choices is essential for blood sugar control.
Best Gluten-Free Whole Grains
- Quinoa: Complete protein with low glycemic impact
- Brown rice: Fiber-rich and versatile
- Buckwheat: Despite the name, it’s gluten-free and highly nutritious
- Oats: Certified gluten-free oats are excellent for stable energy
- Millet: Ancient grain with good fiber content
Practical Tips for Managing Gluten and Blood Sugar
Always Pair Carbohydrates Strategically
Never eat carbohydrates alone. Combine them with:
- Protein (chicken, fish, tofu, legumes)
- Healthy fats (avocado, nuts, olive oil)
- Fiber-rich vegetables (broccoli, spinach, peppers)
This combination slows digestion and prevents blood sugar spikes, whether your meal contains gluten or not.
Monitor Your Individual Response
Everyone’s body responds differently to foods. Use a Dexcom G7 continuous glucose monitor to understand how specific foods affect YOUR blood sugar. What works for someone else may not work for you.
Focus on Whole Foods First
Build your diet around naturally gluten-free whole foods:
- Fresh vegetables and fruits
- Lean proteins
- Legumes and lentils
- Nuts and seeds
- Healthy oils
This approach benefits everyone with diabetes, regardless of gluten status.
What an endocrinologist recommends: Always focus on a low glycemic meal. If you do not know, here is the guide on low glycemic food that helps you to manage your glucose level with proven results.
Conclusion
The relationship between gluten and diabetes is complex and multifaceted. For those with Type 1 diabetes, managing gluten and diabetes is critical if celiac disease is also present. For Type 2 diabetes, the focus should be on overall carbohydrate management and making informed food choices, whether gluten-containing or gluten-free. Understanding how gluten affects your body CGM Devices can help you better control your diabetes and overall health.
Resources






Write a comment
Your email address will not be published. All fields are required