Table of content
- What Is an Insulin Pump?
- How Does an Insulin Pump Work?
- Components of the Insulin Pump and Its Working
- How Algorithms and Automation Assist In Insulin Pump
- How Do Insulin Pumps Work with CGMs?
- Types of Insulin Pumps for Diabetes
- Advantages and Disadvantages of Insulin Pump Therapy
- Conclusion:
- Frequently Asked Question
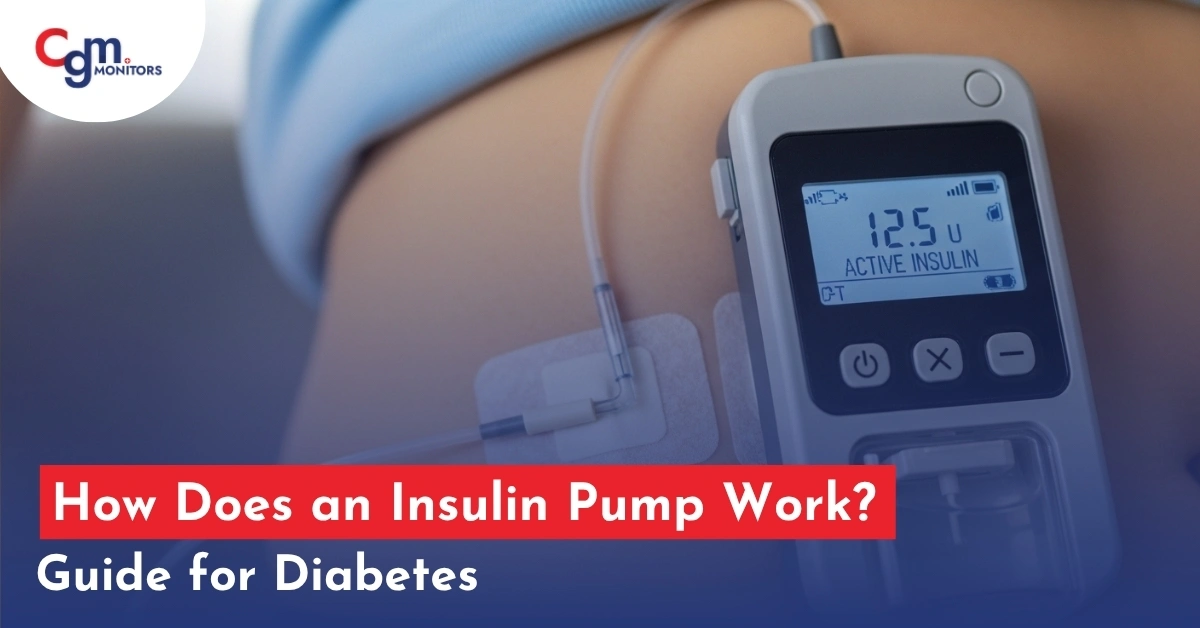
Managing diabetes has come a long way, and one of the most impactful medical devices in recent years is the insulin pump. But one question arises in mind that how does an insulin pump work, and why is it used by both type 1 and type 2 diabetes patients today?
What Is an Insulin Pump?
How Does an Insulin Pump Work?
To answer how an insulin pump works, we break down its two main delivery modes: basal and bolus, along with the internal components and control algorithms.
Basal Insulin Delivery Mode:
- The pump is programmed to deliver small, regular pulses of rapid-acting insulin around the clock, mimicking your pancreas’s natural basal output.
- You can set multiple basal rates throughout the 24-hour day (for example, a higher rate in early morning to counter the dawn phenomenon).
- Many modern pumps (especially when they integrate with CGM) can adjust basal rates automatically based on real-time glucose trends or suspend insulin when glucose is dropping.
Bolus Insulin Delivery Mode:
- When you eat or your glucose is high, you tell the pump the grams of carbohydrate or your current blood sugar. The pump calculates a bolus dose using built-in algorithms (sometimes called a bolus wizard), then you confirm it.
- The bolus is delivered over a short span (seconds to minutes). The pump tracks “insulin on board” (active insulin) to prevent stacking.
- Some pumps allow extended bolus delivery (spread over time), useful for high-fat meals or slow digestion.
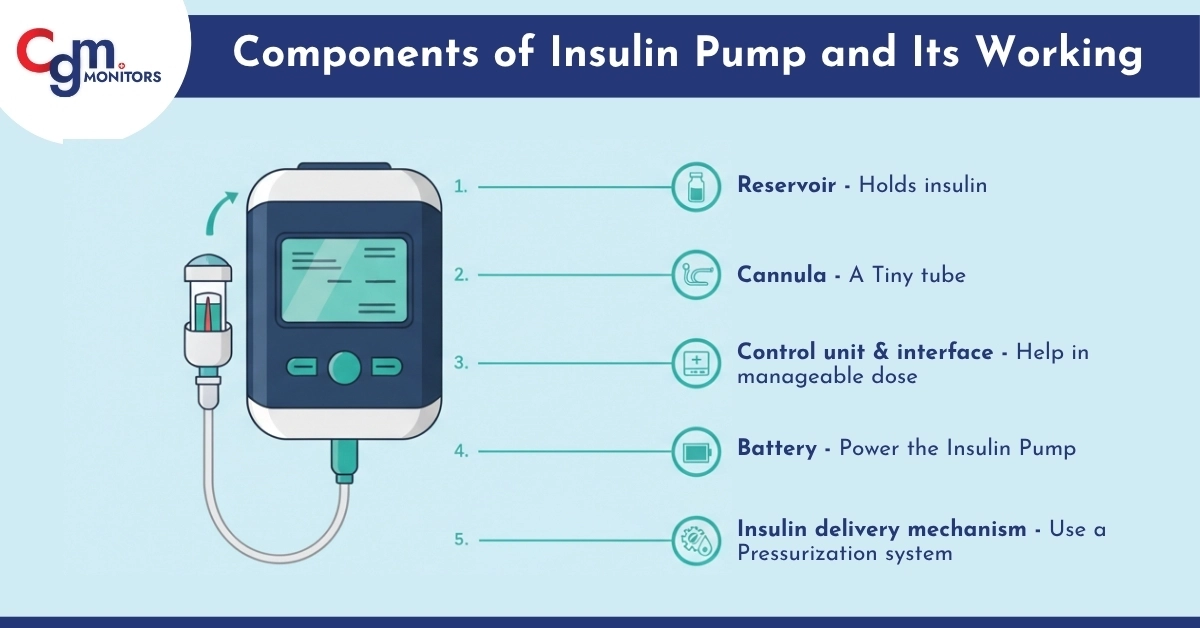
Components of the Insulin Pump and Its Working
To truly grasp how an insulin pump works, let’s peek inside:
- Reservoir: Holds insulin. Replace every 2-3 days.
- Cannula: A Tiny tube that goes under the skin, but the patch insulin pumps are tubeless.
- Control unit & interface: Give you a manageable dose and also alerts.
- Battery: Varies by model; must be monitored. Power the pump.
- Insulin delivery mechanism: Some pumps use a pressurisation system (e.g., pneumatic to deliver insulin.
One Cgm User Summed it Nicely:
All pumps can deliver insulin without a shot every time. Nowadays, many pumps have extra features that help keep your sugar levels in range, like turning off insulin when your sugar is dropping low.
How Algorithms and Automation Assist In Insulin Pump
Modern insulin pumps increasingly use smart algorithms to assist or automate decisions. Key types:
- Open-loop/Sensor-augmented pump: The pump suggests or displays insulin dosing based on user input; the user accepts/adjusts.
- There’s no automatic adjustment.
- Hybrid closed-loop/Automated Insulin Delivery (AID): The pump and CGM interact. The algorithm can increase, decrease, or suspend basal insulin based on glucose trends. But the user still has to input meals/request boluses.
- Full closed-loop (future/experimental): Ideally, the pump/GCM system would fully automate basal + bolus without user meal input. This is a research frontier.
These algorithms rely on predictive modeling (anticipating glucose trends), insulin sensitivity parameters, insulin action curves, and feedback loops to adjust insulin delivery reactively and proactively.
How Do Insulin Pumps Work with CGMs?
Let’s find out how insulin pumps interface with CGM systems (continuous glucose monitors). A CGM (Continuous Glucose Monitor) reads your glucose every few minutes. When connected to your pump:
- The pump adjusts insulin based on real-time glucose data
- Some pumps stop insulin if your sugar is dropping too low
- This creates a “closed-loop system” (also called an artificial pancreas)
If your pump supports integration with our CGM Monitors sensors, the basal algorithm can respond dynamically to real-time glucose data, improving control and reducing hypoglycemia risk.
Types of Insulin Pumps for Diabetes
Understanding the variety of pumps helps you choose what fits your lifestyle. Below are the main categories:
1. Tethered (Tubed) Insulin Pumps
- Use tubing to connect the pump to your infusion site.
- Pros: often more features and larger reservoirs.
- Cons: Tubing can snag, dislodge, or kink.
2. Tubeless Insulin Pump
- The entire device is a pod adhered to your body, no external tubing. Controlled wirelessly by a remote or app.
- Pros: lower obstruction risk, more discreet.
- Cons: you must replace the whole pod every ~2-3 days.
Note: For Type 1 diabetes, devices like the Tandem t:slim X2 are widely used due to their advanced insulin delivery and integration with CGM systems, offering precise control and automation. For Type 2 diabetes, pumps such as the Omnipod 5 G6 pods, provide a flexible, tubeless option that helps those requiring multiple daily injections manage their insulin more conveniently.
Advantages and Disadvantages of Insulin Pump Therapy
Understanding both sides helps users make informed decisions.
Advantages
- Tighter glucose control
- Fewer injections
- Flexibility in meals & lifestyle
- Better handling of dawn phenomenon & basal needs
- Integration with CGM & automation
- Reduced variation/insulin absorption fluctuation
Disadvantages
- Device dependence & technical failure risk
- Skin issues/insertion site problems
- Cost and limited access
- Learning curve/responsibility for management
- Psychological burden/body image
- Rapid risk if insulin delivery is interrupted
Conclusion:
Now you know how insulin pumps work, the different types available, and how they connect with CGM systems. These devices have completely changed the way people manage diabetes by delivering insulin continuously and more precisely, just like a healthy pancreas would.
Whether you have Type 1 or Type 2 diabetes, an insulin pump offers more flexibility, better glucose control, and real-time adjustments when paired with a CGM. With new innovations like hybrid closed-loop systems and tubeless patch pumps, diabetes care is becoming easier, smarter, and more convenient than ever.
Frequently Asked Question
How much does an insulin pump cost, and is it covered by insurance?
Insulin pumps typically cost between $4,000 and $7,000, excluding supplies. Most insurance plans cover pumps with a prescription; check your provider and visit CGM Monitors for options.
Can you swim or shower with an insulin pump?
Many pumps are water-resistant or waterproof, allowing swimming or showering without removal. Always check your pump’s water resistance level and follow manufacturer guidelines
How do you manage insulin pump failures or malfunctions?
If your pump fails, check for alerts, inspect the infusion site, and use backup insulin immediately. Contact your healthcare provider to prevent high blood sugar or complications.
What are the psychological effects of wearing an insulin pump?
Wearing a pump can improve glucose control but may cause body image concerns or anxiety. Support and education help users adjust and feel confident over time.
Can you travel with an insulin pump? Are there any special precautions?
Yes, you can travel with a pump, carry extra supplies and backup insulin. Inform security staff about your device and monitor glucose carefully during trips.
What lifestyle changes are needed when starting an insulin pump?
Pump users must learn to change infusion sites regularly and monitor carbs closely. It offers meal flexibility but requires consistent device management and glucose checks.
How do you handle exercise with an insulin pump?
Exercise may require adjusting basal rates or suspending insulin to avoid lows. Use temporary settings and monitor glucose before, during, and after activity.



Write a comment
Your email address will not be published. All fields are required