Table of content
Swelling in the legs, ankles, or feet is more than just a comfort issue—it can affect mobility, confidence, and overall quality of life. Many people search for exercises for lymph drainage because they are dealing with leg edema, lymphedema, lipedema, or fluid retention, and want a natural, effective way to manage symptoms.
The good news? Exercise is directly associated with an increase in lymph movement, making it one of the most effective non-invasive ways to support lymphatic flow—especially in the lower body.
This guide explains how lymphatic drainage works, why leg-focused movement matters, and the best exercises for lymph drainage that are safe, effective, and evidence-informed.
Understanding the Lymphatic System and Leg Swelling
The lymphatic system is responsible for moving excess fluid, waste products, and toxins out of tissues and back into circulation. Unlike the heart-driven circulatory system, the lymphatic system relies heavily on muscle contraction and movement.
When lymph flow slows down, fluid can accumulate—leading to:
- Swollen legs and feet
- Heaviness or tightness
- Skin changes
- Reduced mobility
This is commonly seen in:
- Lymphedema (primary or secondary)
- Lipedema
- Chronic edema
- Post-surgical or post-cancer recovery
This is where lymphatic system exercises become essential.
Lymphedema has four types based on the four stages. Click on our blog that states the four stages of lymphedema with symptoms and treatments for better understanding.
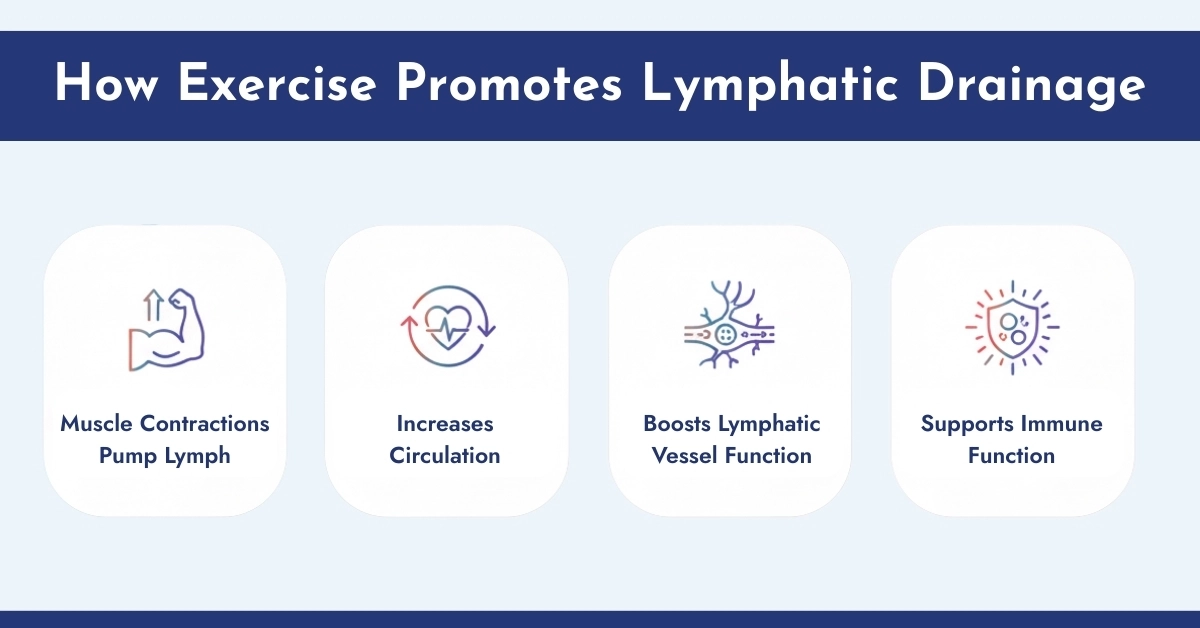
How Exercise Promotes Lymphatic Drainage
The lymphatic system relies on external forces to move lymph fluid. Physical activity stimulates:
- Physical movement and muscle contractions push lymph fluid through the vessels, helping remove waste and toxins from tissues.
- Improves overall blood and lymph circulation, reducing fluid buildup and swelling in areas prone to lymphedema.
- Regular activity strengthens lymphatic vessel walls and valves, making fluid transport more efficient.
- By enhancing lymph flow, exercise helps move immune cells throughout the body, aiding in detoxification and infection prevention.
Best exercises for lymphatic drainage focus on low-impact, controlled movements that facilitate circulation without exacerbating swelling.
Key Exercises for Lymphatic Drainage
- Walking: Encourages calf-muscle pumping and lower limb lymph movement.
- Deep Breathing: Diaphragmatic breathing enhances thoracic duct function.
- Rebounding: Gentle bouncing on a mini-trampoline increases overall lymph flow.
- Stretching: Supports vessel expansion and promotes fluid movement.
- Yoga for Lymphatic Health: Poses such as Legs-Up-the-Wall, Cat-Cow, and Bridge Pose aid full-body drainage.
- Lymphatic Drainage Workouts: Incorporate light cardio, mobility exercises, and gentle resistance to optimize fluid circulation.
Research confirms that exercise is associated with an increase in lymph movement, making it a cornerstone of lymphedema management.
Does Exercise Help Edema and Lymphedema?
The quick and clear answer is Yes—when done correctly. Clinical evidence shows that controlled, low-impact movement improves lymphatic flow, reduces fluid retention, and supports tissue health. The key is choosing the right exercises and avoiding movements that overload or strain the lymphatic system.
Note: It is important to get professionally measured and wear garments as prescribed. Compression garments available on our platform help to reduce lymphedema and help in proper blood flow in the legs and arms. Correct usage supports lymphatic drainage, reduces fluid buildup, and prevents progression of lymphedema.
Why Focus on Legs and Lower Body?
The legs are the most gravity-dependent part of the body. This makes them especially vulnerable to:
- Fluid pooling
- Leg swelling
- Foot and ankle edema
That’s why lymphatic drainage exercises for legs are among the most searched and most recommended interventions for lower-body swelling.
Best Exercises for Lymph Drainage (Legs & Lower Body)
These movements are commonly used in lymphedema physical therapy exercises and are safe for most people when performed gently.
1. Ankle Pumps (Foundation Exercise)
One of the best exercises for lymph drainage and often the first recommended by therapists.
How it helps:
Activates the calf muscle pump, which is crucial for moving lymph and blood upward.
How to do it:
- Sit or lie down with legs elevated
- Slowly point toes away, then pull them back toward you
- Repeat 15–20 times per leg
This is excellent for:
- Foot edema exercises
- Exercises for swollen legs and feet
- Exercises for edema in legs
2. Leg Slides (Heel Slides)
A gentle but effective lymphatic drainage leg exercise.
How it helps:
Encourages fluid movement through the knee and thigh lymph vessels.
How to do it:
- Lie on your back
- Slide one heel toward your buttocks, then back out
- Alternate legs
Ideal for:
- Lymphedema exercises for legs
- Exercises for lymphoedema of the leg
- Post-surgical swelling
3. Seated Marching
Often listed among the top 3 exercises for leg lymphedema.
How it helps:
Engages hip flexors and thigh muscles to stimulate lymphatic flow.
How to do it:
- Sit upright in a chair
- Lift one knee at a time in a slow marching motion
- Keep movements controlled
Great for:
- Exercises to reduce leg swelling
- Leg lymphedema exercises
- Exercises for leg edema
4. Diaphragmatic Breathing (Lymphatic Trigger)
Many people don’t realize that breathing is a lymphatic exercise.
How it helps:
Deep breathing activates the thoracic duct—the main lymph drainage pathway.
How to do it:
- Inhale deeply through the nose, expanding the belly
- Exhale slowly through the mouth
- Repeat for 3–5 minutes
This supports:
- Lymphatic flow exercises
- Exercises to drain the lymphatic system
- Overall lymphatic exercise benefits
5. Gentle Walking
Often underestimated, walking is one of the best exercises for lymphatic drainage.
Why it works:
- Activates multiple muscle groups
- Promotes circulation
- Supports long-term lymph health
Especially helpful:
- To prevent the lymphedema condition and lipedema in the legs.
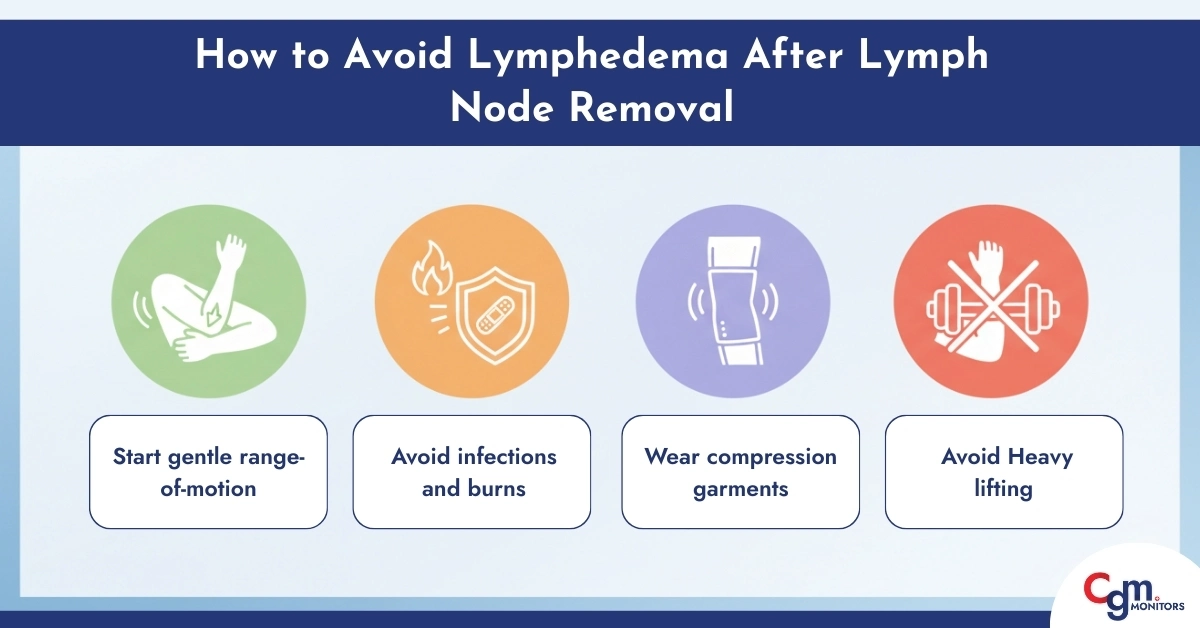
How to Avoid Lymphedema After Lymph Node Removal
People who undergo lymph node dissection (axillary, groin, pelvic, or neck) have a higher risk of developing lymphedema. Preventive exercises and precautions significantly reduce the risk.
Key Prevention
- Start gentle range-of-motion exercises within 1–2 weeks post-surgery (as approved by your doctor).
- Avoid infections, burns, and cuts in the affected limb.
- Maintain a healthy body weight.
- Do deep breathing exercises for the lymphatic system to stimulate lymph flow.
- Wear compression garments for legs (4 chamber) or arms during activity if recommended.
- Avoid heavy lifting in the early healing stages.
Exercises to Avoid With Lymphedema
Not all exercises are safe, especially during early stages or after surgery. Avoid:
Heavy weightlifting without clearance
High-impact arm movements
Hot yoga or overheating activities
Exercises that cause pain or swelling
Tight clothing during workouts
Following these precautions reduces the risk of aggravating lymphedema.
Conclusion
Incorporating lymphedema physical exercise into daily life is critical for fluid management, mobility, and overall well-being. From gentle stretching and deep breathing to guided physical therapy routines and yoga, exercise and lymphatic system health go hand in hand. With proper precautions, compression therapy, and lifestyle adjustments, individuals with lymphedema can lead active, fulfilling lives without compromising safety.
Professional References
- Mayo Clinic — Symptoms & Causes of Lymphedema
- American Cancer Society — Lymphedema (overview & treatment)
- Cleveland Clinic — Lymphedema Overview
Disclaimer:
This guide provides general information about diabetes-friendly seafood but is not a substitute for professional care. Always follow your doctor’s advice. Some images in this article are AI-generated to aid understanding.
Frequently Asked Questions
What is the best exercise for lymphedema?
The best exercises for lymphedema are gentle, low-impact movements that stimulate lymph flow without causing strain. Walking, swimming, yoga, deep breathing, and range-of-motion exercises help reduce swelling, improve circulation, and maintain flexibility. Start slowly and increase intensity gradually while monitoring for any swelling or discomfort.
How to treat lymphedema in the breast?
Breast lymphedema can be managed with a combination of manual lymphatic drainage (MLD), compression garments, gentle arm and chest exercises, and physical therapy. Consistent care helps prevent fluid buildup, relieve heaviness, and reduce discomfort while maintaining mobility in the affected area.
Which sleeping position is best for lymphatic drainage?
For optimal lymphatic drainage, elevate the affected limb slightly above heart level using pillows. This position encourages fluid to flow back toward lymph nodes, reducing swelling overnight. Avoid positions that put pressure on swollen areas, and change positions gently to maintain comfort.
What is the gold standard treatment for lymphedema?
Complete Decongestive Therapy (CDT) is considered the gold standard for lymphedema management. It combines manual lymphatic drainage, compression therapy, targeted exercises, skin care, and education to reduce swelling, prevent infection, and improve quality of life.
What foods should you avoid if you have lymphedema?
Limit processed foods, excess salt, sugary drinks, and saturated fats, which can worsen fluid retention. Focus on a balanced diet rich in fruits, vegetables, lean protein, and anti-inflammatory foods to support lymphatic health and reduce swelling.
What is a good home remedy for lymphedema?
Effective home remedies include gentle exercises, elevation of affected limbs, light massage, proper hydration, wearing compression garments, and maintaining a healthy weight. While home care cannot cure lymphedema, it can help manage symptoms and prevent worsening of swelling.
Can compression garments make lymphedema worse?
Improperly fitted compression garments may worsen swelling or restrict blood flow. It is important to get professionally measured and wear garments as prescribed. Correct usage supports lymphatic drainage, reduces fluid buildup, and prevents progression of lymphedema.



Write a comment
Your email address will not be published. All fields are required