Table of content
- Understanding the Link Between Sleep and Blood Sugar
- Why Sleep Is Vital for Diabetic Health
- How Sleep Affects Glucose Regulation
- Common Sleep Problems in People with Diabetes
- Practical Sleep Tips for Diabetics
- Continuous Glucose Monitors (CGM) and Sleep
- When to Consult Your Healthcare Provider
- Final Thoughts
- Frequently Asked Questions
Did you know that poor sleep over the years, especially for night duty personnel, may increase your risk of obesity, cardiovascular problems and diabetes? Your sleep habits aren’t just about feeling rested—they have a direct impact on your blood sugar levels. For people with diabetes, understanding the link between sleep and glucose control is essential for maintaining health and preventing complications.
This guide explains how sleep patterns and diabetes are linked, how it affects blood sugar, common sleep problems in diabetes, and how tools like continuous glucose monitoring (CGM) devices can help you manage your glucose while sleeping.
Key Takeaways
- Sleep disorders, including sleep apnea and restless leg syndrome, can worsen blood sugar control.
- Maintaining 7–9 hours of core sleep per night is essential for diabetic health.
- Sleep patterns and circadian rhythms play a crucial role in glucose regulation and insulin sensitivity.
- Sleep deprivation can increase insulin resistance and raise blood sugar levels.
- People with pre-diabetes or diabetes often experience poorer sleep quality compared to individuals with normal glucose levels.
- Using CGM monitors like the new Dexcom G7 sensor can provide insights into how sleep affects glucose levels and help prevent nighttime highs and lows.
Understanding the Link Between Sleep and Blood Sugar
The relationship between sleep and blood sugar is very complex due to psychological behaviour and patterns. During sleep, your body undergoes physiological changes that influence glucose regulation. Poor sleep can disrupt these processes, leading to higher blood sugar levels and insulin resistance.
For example, the “dawn phenomenon” occurs between 4–8 a.m., causing a natural rise in blood sugar due to the body’s overnight release of hormones like growth hormone, cortisol, and glucagon that prepare you to wake up. In healthy individuals, insulin keeps glucose under control. In people with diabetes, insulin may not work as efficiently, leading to higher fasting glucose levels.
By maintaining good sleep habits and monitoring your glucose, you can reduce the effects of insulin resistance and improve overall blood sugar control.
Why Sleep Is Vital for Diabetic Health
Quality sleep helps your body:
- Maintain healthy insulin function
- Support glucose metabolism
- Reduce the risk of diabetes-related complications
Sleep disorders like sleep apnea are particularly common in type 2 diabetes, increasing insulin resistance and making glucose management more difficult. Studies show that treating sleep issues can significantly improve blood sugar levels and overall health.
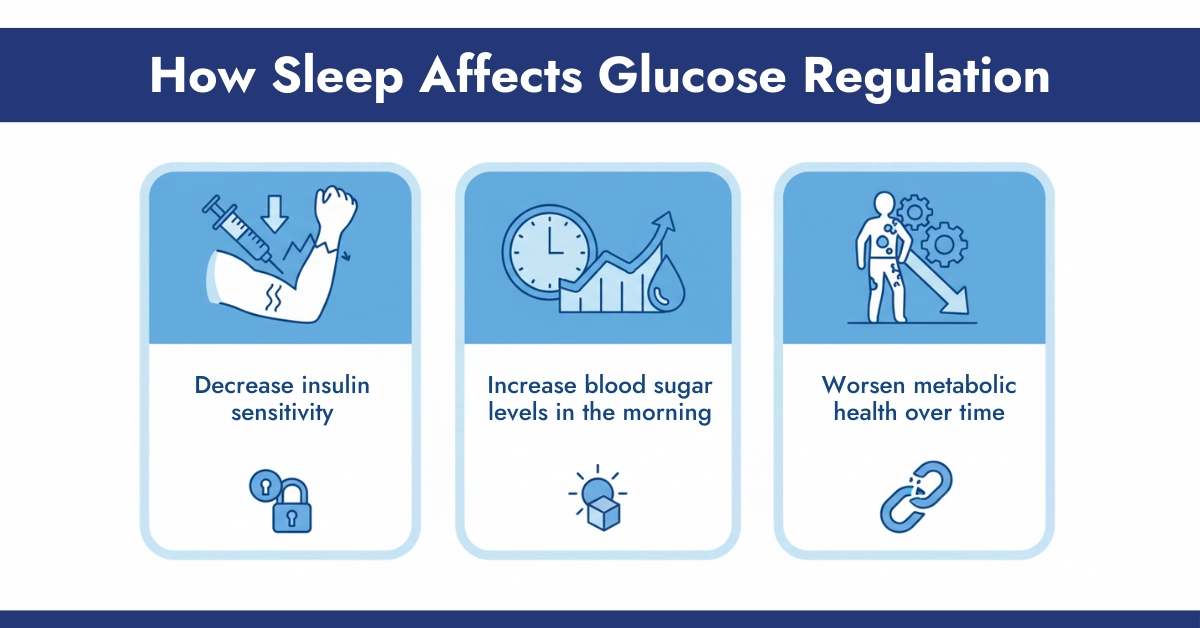
How Sleep Affects Glucose Regulation
Research indicates that sleep deprivation can:
- Decrease insulin sensitivity by 25–30% within a few days
- Increase blood sugar levels in the morning
- Worsen metabolic health over time
Conversely, improving sleep in people with short sleep duration can boost insulin sensitivity, helping maintain more stable blood sugar throughout the day.
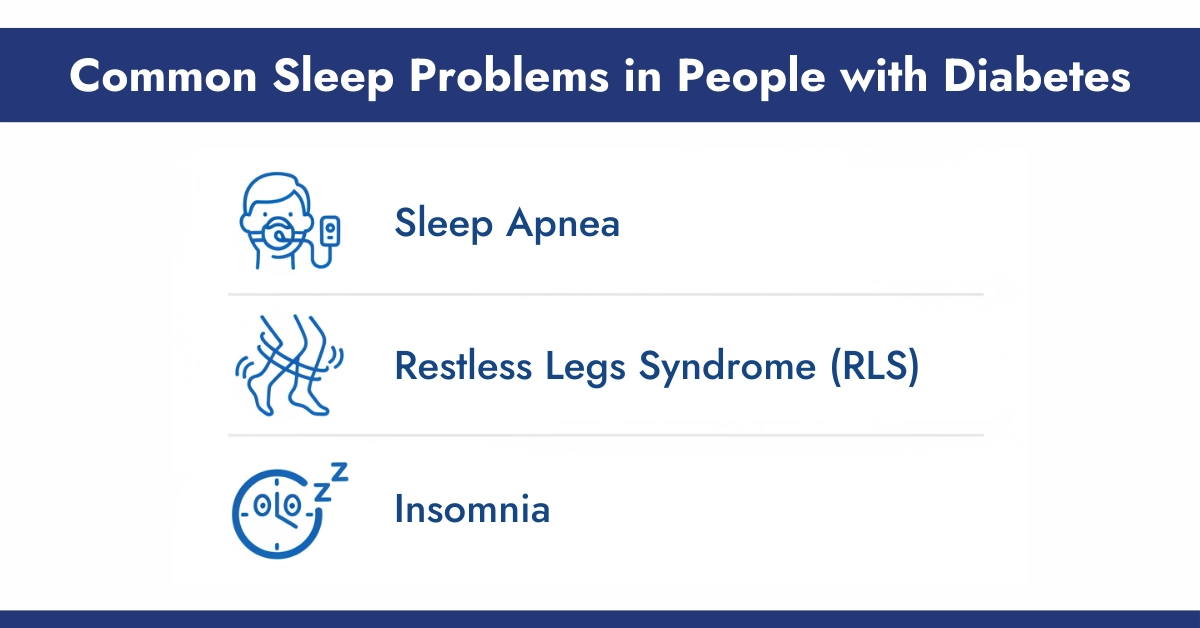
Common Sleep Problems in People with Diabetes
People with diabetes are more likely to experience sleep disorders, including:
Sleep Apnea
- Up to two-thirds of type 2 diabetics may have sleep apnea.
- Interrupted breathing at night worsens insulin resistance.
- Using CPAP therapy can lower morning glucose levels by approximately 12 mg/dL in type 2 diabetes patients.
Restless Legs Syndrome (RLS)
- Causes uncomfortable sensations in the legs, disrupting sleep.
- Common in diabetics due to high blood sugar and nerve damage.
- Proper management improves both sleep quality and glucose control.
Insomnia
- Difficulty falling or staying asleep can increase stress hormones, raising blood sugar levels.
- Chronic insomnia may increase the risk of type 2 diabetes over time.
Practical Sleep Tips for Diabetics
Create a Sleep-Friendly Environment
- Keep the bedroom cool, dark, and quiet (65–70°F / 18–21°C).
- Use blackout curtains or an eye mask to block light.
- Reduce noise with earplugs or a white noise machine.
- Invest in a supportive mattress and comfortable pillows.
Follow Good Sleep Hygiene
- Stick to a regular sleep schedule, even on weekends.
- Avoid screens at least one hour before bedtime.
- Engage in relaxing activities: reading, warm baths, stretching, or meditation.
- Monitor blood sugar before bed and adjust meals or medication if needed.
Continuous Glucose Monitors (CGM) and Sleep
CGM devices, such as the Freestyle Libre 2 Plus and 3 Plus, are revolutionary for people with diabetes. They track glucose levels continuously, providing critical insights into how sleep patterns affect blood sugar.
Benefits of CGM During Sleep
- Detects nighttime high or low glucose levels
- Helps prevent dangerous nocturnal hypoglycemia or hyperglycemia
- Allows adjustments to medication, diet, or bedtime routines
- Provides data to identify patterns between sleep quality and glucose fluctuations
A study of 28 type 2 diabetes patients monitored over 249 days of glucose tracking and 221 nights of sleep showed that sleep timing and quality directly influenced glucose stability. Sleeping later or inconsistently made blood sugar more unpredictable, while consistent, adequate sleep improved glucose control.
Using CGM for Better Diabetes Management
- Tracks glucose continuously without frequent fingersticks
- Offers alerts for high or low glucose during sleep
- Helps both patients and healthcare providers make informed decisions
- Integrates with sleep tracking apps to correlate sleep and glucose patterns
By combining CGM data with good sleep habits, diabetics can take proactive steps to stabilize glucose levels and reduce the risk of complications.
Understanding how overall sleep affects blood sugar is only part of the picture. To manage diabetes effectively, it’s also important to focus on core sleep, the deep sleep stages that play a critical role in insulin sensitivity and glucose regulation. Our next guide explores core sleep and how diabetics can optimize it for better health.
When to Consult Your Healthcare Provider
Consult a healthcare provider if you notice:
- Morning blood sugar is consistently high.
- Excessive daytime fatigue despite adequate sleep.
- Suspected sleep apnea or restless legs syndrome.
For type 1 diabetics, CGM systems and hybrid closed-loop devices can reduce nighttime hypoglycemia and improve overall sleep quality. For type 2 diabetics, sleep interventions like CPAP therapy or lifestyle modifications can enhance glucose control.
Final Thoughts
Sleep and diabetes are deeply interconnected. Poor sleep can worsen insulin resistance and destabilize blood sugar levels, while quality sleep supports glucose regulation and overall health. By practising good sleep hygiene, addressing sleep disorders, and using CGM monitors, people with diabetes can better manage their blood sugar, reduce complications, and improve their quality of life.
Making sleep a priority is a vital part of any diabetes management plan. With the right combination of habits, medical guidance, and technology like CGM, you can achieve better blood sugar stability and long-term metabolic health.
Frequently Asked Questions
How does one night of poor sleep affect blood sugar in diabetics?
Even a single night of poor sleep can increase morning blood sugar up to 200 mg/dL and reduce insulin sensitivity for the next day.
Can better sleep reduce diabetes medication needs?
While sleep alone doesn’t replace medication, improving sleep can enhance insulin efficiency and may reduce the required dosage over time.
What is the ‘dawn phenomenon’?
It’s the early morning rise in blood sugar due to hormones. Poor sleep worsens this effect, leading to higher fasting glucose levels.
Which sleep disorders affect diabetics most?
Sleep apnea and restless legs syndrome are more common in diabetics and can worsen glucose control.
How can CGM help with nighttime blood sugar issues?
CGM devices like libre 3 Plus track glucose continuously, alerting users to highs and lows and helping adjust medications or bedtime routines for better overnight glucose management.




Write a comment
Your email address will not be published. All fields are required