Table of content
It is widely accepted and used in clinical guidelines and hospital order sets.The weight based insulin dosing is a method that calculates insulin doses according to a person’s body weight, typically in units per kilogram (U/kg) instead of a fixed dose. The method helps tailor dosing more accurately, especially at the initiation of insulin therapy, and may result in better glycemic control with less hypoglycemia than flat doses, if carried out carefully.
What is Weight-Based Insulin Dosing?
Insulin is a life-saving therapy for millions of people living with diabetes, but finding the correct dose can be tricky. Too little insulin leads to high blood sugar, while too much increases the risk of hypoglycemia. Traditionally, some patients were started on a fixed insulin dose, regardless of their weight or insulin sensitivity.
This method is widely used because it provides:
- A standardized starting point for patients
- Clinically accurate dosing
- A reduced risk of hypoglycemia
- A personalized approach to insulin therapy
It is especially useful for:
- Newly diagnosed Type 1 diabetes
- Insulin-dependent Type 2 diabetes
- Hospitalized patients under glucose control
- Transitioning from oral medications to insulin
- Setting initial insulin pump parameters
This method is supported by ADA (American Diabetes Association) guidelines and remains a gold standard in modern diabetes care.
Weight-Based vs. Fixed Dosing
The key difference between fixed and weight-based insulin dosing lies in personalization.
- Fixed dosing: A standard dose is prescribed to most patients, such as 10 or 20 units per day. This may be simple but often fails to consider weight, insulin resistance, or kidney health.
- Weight-based dosing: Insulin needs are calculated according to body weight, creating a tailored plan that minimizes the risk of under- or overdosing.
Study Highlight: In a trial of people with Type 2 diabetes and renal insufficiency, researchers compared 0.5 U/kg/day vs. 0.25 U/kg/day using glargine and glulisine. Both groups achieved similar average glucose (~174 mg/dL), but hypoglycemia occurred in 30% of patients at 0.5 U/kg/day vs. 15.8% at 0.25 U/kg/day.
Formulas for Weight-Based Insulin Dosing
Total Daily Dose (TDD) Formula: TDD = 0.4 to 0.6 units × body weight (kg). When calculating insulin doses, several formulas and safe ranges are recommended:
- Type 2 diabetes (outpatient start): ~0.3 U/kg/day
- Renal-impaired inpatients: 0.25–0.5 U/kg/day
- Safe upper limit: ≤0.6 U/kg/day (above this, hypoglycemia risk rises significantly)
- Acute hyperkalemia: 0.1 U/kg IV insulin is safer than a flat 10-unit dose
This range varies based on insulin resistance, age, and diabetes type:
| Type of Patient | Recommended Units/kg/day |
|---|---|
| Newly diagnosed Type 1 diabetes | 0.4–0.5 U/kg |
| Lean adults | 0.4 U/kg |
| Average-weight adults | 0.5 U/kg |
| Insulin-resistant adults | 0.6–0.8 U/kg |
| Obese adults | 0.7–1.0 U/kg |
These ranges are based on clinical studies and endocrinology treatment standards.
Still pricking fingers? Pricking fingers is no longer required just to check blood glucose. Continuous glucose monitors (CGMs) monitor your glucose data 24/7, and most of the latest ones, such as Freestyle Libre 2 Plus Sensors, are automatic insulin delivery (AID) compatible as well.
Weight-Based Insulin Dosing Chart
This chart provides a simplified reference for clinicians and patients:
| Body Weight (kg) | TDD (0.5 U/kg) | Basal Dose (50%) | Bolus Dose (50%) |
|---|---|---|---|
| 50 kg | 25 U | 12 U | 13 U |
| 60 kg | 30 U | 15 U | 15 U |
| 70 kg | 35 U | 17 U | 18 U |
| 80 kg | 40 U | 20 U | 20 U |
| 90 kg | 45 U | 22 U | 23 U |
| 100 kg | 50 U | 25 U | 25 U |
This chart is for initial estimations. Actual doses must be fine-tuned based on glucose readings and medical evaluation.
Common Mistakes and Safety Risks
Weight-based dosing is effective, but safety must always come first. Here are key precautions:
- Start low: Use 0.25–0.4 U/kg/day for underweight patients or those with kidney disease.
- Avoid exceeding 0.6 U/kg/day: Higher doses increase the chance of hypoglycemia.
- Monitor daily glucose: Especially important during initiation or dose changes.
- Educate patients: Teach proper injection techniques, site rotation, and signs of hypoglycemia.
Did you know? Metformin, often prescribed for Type 2 diabetes, can help offset insulin-related weight gain when used together with insulin therapy. Let s explore how metformin helps you to lose weight in a few months.
Monitoring Insulin Therapy: The Role of CGMs
Traditional self-monitoring with finger pricks is useful but often inconvenient. Thankfully, Continuous Glucose Monitors (CGMs) now provide real-time glucose tracking without constant fingersticks.
Benefits of CGMs in Weight-Based Dosing
- Predict and prevent hypoglycemia: Some CGMs, such as the Dexcom G7, provide alerts before glucose levels drop too low.
- Track glucose trends: Allows better basal and bolus insulin adjustments.
- Improve safety during activity and sleep: Reduce overnight lows and exercise-related hypoglycemia.
- Data sharing with providers: CGM reports can be reviewed remotely, ensuring personalized adjustments.
Modern CGMs like Freestyle Libre 3 Plus Sensors and Dexcom G7 are also compatible with many automated insulin delivery (AID) systems, making weight-based insulin dosing even more precise.
Key Terms and Formulas
| Term | Typical Value / Formula | Notes |
| TDD starting dose | 0.3 U/kg/day | Type 2 outpatient |
| Renal-impaired inpatient | 0.25–0.5 U/kg/day | Safer range |
| Safe upper limit | 0.6 U/kg/day | Beyond raises hypo risk |
| Acute hyperkalemia dose | 0.1 U/kg IV | Safer than a flat dose |
Final Takeaways
- Weight based insulin dosing is considered safer and more effective than fixed dosing for many people with diabetes. Furthermore, to avoid hypoglycemic (low sugar) events, CGM systems may help.
- While initiating insulin therapy, 0.3 U/kg/day may be the best; afterwards, remember that doses under the 0.6 U/kg/day threshold reduce hypoglycemia risk. Weight changes should prompt dose reassessment.
- With regular monitoring and adjustments, weight-based dosing facilitates precise insulin therapy, minimizes adverse events, and empowers people living with diabetes to lead healthier lives.
Frequently Asked Questions
What is weight-based insulin dosing for diabetics?
Weight-based insulin dosing calculates a patient’s total daily insulin needs using body weight in kilograms. The dose is then split into basal and bolus portions. This method personalizes therapy, starts conservatively, and is refined through ongoing glucose monitoring.
How do I calculate initial insulin doses based on body weight?
Initial total daily dose (TDD) is usually 0.4–0.5 units/kg for type 1 diabetes or 0.2–0.3 units/kg (or a fixed 10 units) for insulin-naive type 2 patients. Higher ranges up to 1.0 units/kg may be used with insulin resistance. Split TDD about 50% basal and 50% bolus, then titrate based on glucose trends.
How to calculate insulin dose per kg?
Multiply body weight in kilograms by 0.2–1.0 units/kg/day depending on diabetes type and insulin resistance. This gives the total daily dose, which is typically divided evenly between basal and bolus insulin, then fine-tuned using glucose data.
Why is weight an important factor in insulin dosage?
Body weight closely correlates with insulin needs because higher body mass—especially excess fat—increases insulin resistance. Weight provides a reliable starting point that reflects metabolic demand better than fixed doses, and dose needs change as weight changes.
Impact of obesity on insulin resistance and dosing?
Obesity increases insulin resistance through inflammatory cytokines and free fatty acids, impairing insulin signaling in tissues. This often raises insulin requirements, sometimes above 1 unit/kg/day. Weight loss can significantly reduce resistance and lower insulin needs.
What are the advantages of using weight-based insulin dosing?
It provides a personalized, evidence-based starting point that reduces the risk of under- or overdosing. Weight-based dosing supports safer titration, faster glycemic control, and lower hypoglycemia risk compared to fixed-dose approaches.
What factors besides weight influence insulin dosing adjustments?
Blood glucose patterns, carbohydrate intake, illness, stress, medications, physical activity, hormones, age, kidney or liver function, and injection sites all affect insulin needs. Regular monitoring helps tailor doses precisely.
Why is it crucial to monitor blood glucose closely with weight-based insulin?
Weight-based doses are estimates. Frequent glucose monitoring helps prevent hypoglycemia or hyperglycemia, guides safe titration, reveals daily patterns, and ensures long-term effectiveness—especially when paired with CGM use.
Who can benefit most from a weight-based insulin dosing approach?
People with type 2 diabetes starting insulin, patients with obesity-related insulin resistance, hospitalized individuals, and those transitioning therapies benefit most. Overall, most insulin users gain from this structured, adaptable approach under medical guidance.
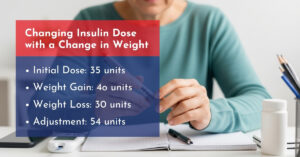
How can I adjust my insulin dose if my weight changes significantly?
Recalculate the total daily dose using the new weight and per-kg guidelines, then adjust basal and bolus doses accordingly. Make gradual changes (10–20%), monitor glucose closely, and consult your healthcare provider to account for activity or diet changes.
How does exercise impact insulin requirements with weight-based dosing?
Exercise improves insulin sensitivity, often reducing insulin needs during and up to 24 hours after activity by 10–50%. Intense exercise may temporarily raise glucose due to stress hormones. Frequent monitoring helps guide safe dose adjustments.
Disclaimer: This blog is only for informational purposes. Always check with your healthcare specialist before taking any medical action.


Write a comment
Your email address will not be published. All fields are required