Table of content
Maintaining normal blood sugar levels is crucial for everyone. People with diabetes are more vulnerable to irregular sugar levels. Therefore, to prevent complications related to high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia), regular glucose monitoring is necessary. Dangerous blood sugar levels can lead to severe health issues, including life-threatening ones, and understanding what constitutes these levels is key to managing diabetes effectively and wondering, ‘What Level of Blood Sugar is Dangerous?. In this comprehensive guide, we’ll explore normal, risky, and emergency blood sugar levels, their causes, symptoms, and strategies for prevention and management.
Understanding Blood Sugar Levels
Blood sugar, or glucose, is the primary source of energy for your body. It is influenced by diet, physical activity, medications, and underlying health conditions such as diabetes. Understanding what constitutes a safe blood sugar range is key to preventing complications.
- Normal fasting blood sugar: 70–99 mg/dL
- Normal post-meal blood sugar: Less than 140 mg/dL
- Prediabetes range: 100–125 mg/dL fasting, 140–199 mg/dL post-meal
Monitoring your blood sugar regularly can help you maintain safe glucose levels and detect potential risks early.
Blood sugar levels above 180 mg/dL (after eating) and above 130 mg/dL (during fasting) are considered high. And levels below 70 mg/dL or above 300 mg/dL are dangerous.
Different Types of Blood Sugar Levels
Blood sugar levels can vary throughout the day depending on when you eat and how much physical activity you engage in. The following table shows how blood sugar levels relate to potential medical emergencies:
| Blood Sugar Level (mg/dL) | Risk Level |
| Below 70 | High risk (hypoglycemia) |
| 70 – 100 | Low risk (normal) |
| 100 – 125 | Moderate risk (prediabetes) |
| Above 126 | High risk (diabetes) |
| 180+ | Very high risk (hyperglycemia) |
| 400+ | Extreme danger (diabetic crisis) |
Did you know?
Continuous glucose monitors (CGMs) monitor your glucose levels 24/7 without you needing to even prick your fingers, give high and low alerts, and some of the latest ones, like Freestyle Libre 2 Plus Sensors, can be integrated with automatic insulin delivery systems as well.
Dangerous Blood Sugar Levels – High and Low
1. Low Blood Sugar (Hypoglycemia)
Hypoglycemia occurs when blood sugar drops below safe limits. Low blood sugar can be dangerous and even fatal if untreated.
Symptoms of Low Blood Sugar (Hypoglycemia)
When blood sugar levels fall too low, below 70 mg/dL, it can lead to hypoglycemia, which can be dangerous if not treated quickly. Symptoms include:
- Shakiness
- Sweating
- Irritability
- Confusion
- Dizziness or lightheadedness
- Weakness
- Blurred vision
- Loss of consciousness (in severe cases)
In extreme cases, dangerously low blood sugar levels can lead to seizures, coma, and even death. People with diabetes should always carry a quick source of sugar (like glucose tablets) to raise blood sugar in case of hypoglycemia.
2. High Blood Sugar (Hyperglycemia)
Hyperglycemia occurs when blood glucose rises above the normal range. Persistent high blood sugar can damage organs, nerves, and blood vessels.
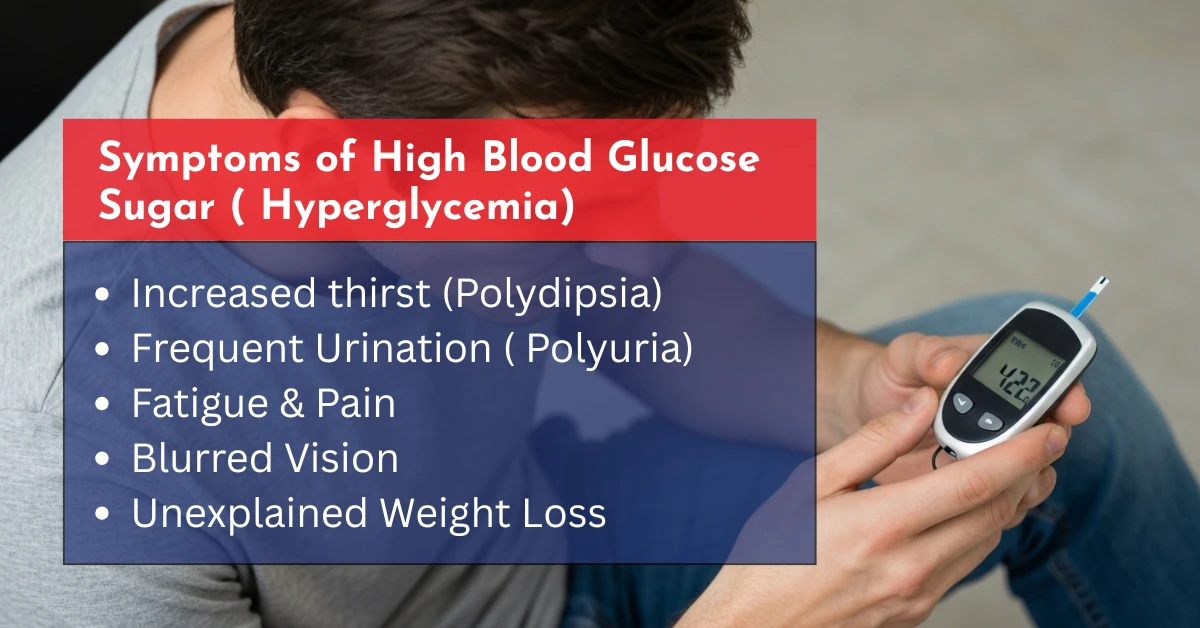
Symptoms of High Blood Sugar (Hyperglycemia)
Hyperglycemia occurs when blood sugar goes too high, generally above 180 mg/dL.
Common indicators of elevated levels:
- Increased Thirst (Polydipsia): Excess glucose in the bloodstream leads to fluid loss through urine, causing dehydration and heightened thirst.
- Frequent Urination (Polyuria): The kidneys work to eliminate excess glucose, resulting in more frequent urination.
- Fatigue: High blood sugar impairs the body’s ability to utilise glucose for energy, leading to feelings of tiredness.
- Blurred Vision: Elevated glucose levels can cause fluid to shift into the eye lenses, affecting focus.
- Unexplained Weight Loss: When cells can’t access glucose, the body starts breaking down muscle and fat for energy.
- Slow-Healing Sores: High blood sugar can impair the body’s natural healing processes.
- Increased Hunger (Polyphagia): Despite high blood sugar levels, cells may not get enough glucose, triggering hunger.
- Dry Mouth and Skin: Dehydration due to fluid loss can lead to dry mouth and skin.
- Numbness or Tingling in Hands or Feet: Chronic high blood sugar can lead to nerve damage, known as diabetic neuropathy.
Causes of Dangerous Blood Sugar Levels
Several factors contribute to dangerous blood sugar levels, including both hyperglycemia and hypoglycemia. Understanding the causes helps in prevention.
- Diabetes type 1 and 2: The most common cause of blood sugar extremes
- Insulin overdose or improper medication: Can cause severe hypoglycemia
- Skipping meals or a poor diet: Lowers blood sugar unexpectedly
- Stress, illness, or infection: Can elevate blood sugar
- Certain medications: Steroids, diuretics, or beta-blockers may influence glucose levels
Want to claim a CGM sensor?
With CGM Monitors, it’s easy to claim a CGM using insurance or buy one using your debit/credit card. Get a free eligibility check now.
Management of Blood Sugar Levels
The blood sugar levels shared by the Mayo Clinic have been recommended by the American Diabetes Association (ADA) for diabetic people.
Blood Sugar Monitoring
Use a glucometer or CGM Sensor (used for continuous monitoring without fingerpricking) to check your blood sugar levels.
- Before meals: Target blood sugar level is typically 70–130 mg/dL.
- After meals: After 1-2 hours of meals, blood sugar should be less than 180 mg/dL.
- Fasting blood sugar: Should generally be 80–130 mg/dL.
- Postprandial (2 hours after eating): A blood sugar level of less than 180 mg/dL is typically safe.
Dietary Adjustment
- For most adults with diabetes, it’s recommended to aim for 45-60 grams of carbohydrates per meal.
- For the best packaged snacks, try to keep your carbohydrate intake between 15-30 grams.
- You can use the carbohydrate-to-insulin ratio (e.g., 1 unit of insulin for every 15 grams of carbohydrates) to help adjust insulin doses.
- Focus on complex carbohydrates (like whole grains, beans, and vegetables) as they release sugar more slowly into the bloodstream.
Insulin Management:
- If you’re on insulin, adjust your dosage according to your blood sugar readings. For example, if your fasting blood sugar is 116 mg/dL, you might need an adjustment in your insulin dosage.
Insulin sensitivity factors can help you calculate how much insulin is needed to lower your blood sugar by a certain amount (e.g., 1 unit of insulin lowers blood sugar by 30 mg/dL).
- Use an insulin dose chart provided by your healthcare provider to match insulin doses with carbohydrate intake.
Exercise and Lifestyle
- Aim for 150 minutes of moderate-intensity aerobic exercise per week, which is about 30 minutes a day, 5 days a week. You must adopt home-based effective exercise daily.
- Physical activity helps increase insulin sensitivity, meaning your body can use insulin more effectively and lower blood sugar.
- If you have high blood sugar (e.g., >240 mg/dL), check your urine for ketones before exercising, as exercising with high ketones can be dangerous.
For insulin therapy, it’s important to follow an insulin dose chart provided by your healthcare team. The amount of insulin needed varies depending on factors like activity level, food intake, and current blood sugar levels.
Emergency Treatment
- For low blood sugar: use glucose tablets like True Plus, or glucagon injections if severe
- For high blood sugar: hydrate, check ketones, and contact your healthcare provider
When to Seek Medical Help
Prompt recognition of dangerous blood sugar levels is essential to prevent severe complications. Seek immediate medical attention if you experience:
- Extremely high blood sugar (>300 mg/dL) accompanied by nausea, vomiting, or abdominal pain.
- Severe low blood sugar (<54 mg/dL) with symptoms like confusion or loss of consciousness.
- Persistent high or low glucose levels despite dietary or lifestyle adjustments.
- Symptoms of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), such as rapid breathing, fruity breath, or extreme fatigue.
Conclusion:
Blood glucose levels below 70 mg/dL or above 180 mg/dL require emergency medical care. Lifestyle changes can help you manage healthy blood sugar levels. These changes include a balanced diet, regular exercise, proper sleep, regular glucose monitoring, and medication (when prescribed). People with high blood sugar issues may find it useful to use an automatic insulin delivery system, such as an Omnipod 5. These AID systems take away the distress of multiple injections and minimise the chances of adverse events.
To prevent complications, consider getting diet plans from a certified professional, exercise regularly, sleep properly, and don’t stress much. Remember, prevention is better than a cure.




Write a comment
Your email address will not be published. All fields are required