Table of content
- Role of Insulin: How it Affects
- Insulin Types and How They Work
- Will Insulin Kill a Non Diabetic Person?
- Is There a Fatal Dose of Insulin for Non-Diabetics?
- What Should I do If Someone Injects Insulin By Mistake?
- Emergency Treatment for Insulin Poisoning
- Why Non-Diabetics Should Never Use Insulin
- Preventing Accidental Insulin Injections
- Real-Life Scenarios & Tools That Could Have Helped
- Death by Insulin: A Worst Scenario Ever
- Conclusion
- Frequently Asked Questions
Insulin is one of the most important medications in modern healthcare. For people with type 1 diabetes and many with type 2 diabetes, insulin therapy is life-saving. It helps regulate blood sugar and prevents dangerous complications. So, will insulin kill a non diabetic person? Yes, if insulin overdoses. An overdose can trigger life-threatening hypoglycemia, seizures, coma, or death due to insulin. Fast intervention can save a life. In this article, we’ll explore how insulin works, what happens when a non diabetic takes insulin, signs of overdose, treatment options, and expert recommendations.
Role of Insulin: How it Affects
Natural insulin is just a hormone that regulates blood sugar. It does so by storing and moving glucose from the bloodstream into cells for energy. For diabetics, this natural system is weakened or diminished. Type 1 patients produce no insulin, while Type 2 patients cannot utilise the insulin they produce efficiently. In both cases, injected insulin helps control glucose levels.
But what happens if you take insulin without diabetes? The body already produces what it needs, so it can be risky if it’s in large amounts. However, not all insulins affect diabetics the same way; it changes the risk factor in non-diabetics as well. To understand that risk, it’s useful to know how each insulin type works:
Insulin Types and How They Work
| Type | Onset | Peak | Duration | Examples |
| Rapid-Acting | 10-15 mins | 30 min-2 hrs | 4-6 hrs | Lispro, Aspart, Glulisine |
| Short-Acting | ~30 mins | 2–3 hrs | 3-6 hrs | Regular (R) insulin |
| Intermediate-Acting | ~2 hrs | 4-12 hrs | 12-18 hrs | NPH (N) insulin |
| Long-Acting | 1-2 hrs | No peak | 20-24 hrs | Glargine, Detemir |
Will Insulin Kill a Non Diabetic Person?
The direct answer: Yes, insulin can kill a non diabetic person if injected in sufficient quantity. When someone without diabetes takes insulin, blood sugar levels may drop too far, a condition known as hypoglycemia. Even small amounts of injected insulin can be harmful to healthy individuals, and misuse should never be attempted.
What Happens If a Non-diabetic Takes Insulin:
Taking insulin without having diabetes can be extremely dangerous for a non-diabetic person. Insulin’s main role is to lower blood sugar, and in someone with normal glucose levels, it can cause severe imbalances. However, this compensation is time-limited. If blood glucose keeps falling, symptoms worsen quickly. Here’s what’ll happen if a non diabetic takes insulin:
- Blood glucose will fall quickly (hypoglycemia)
- Tremors, shaking or coma
- Weight gain
- Excessive sweating
- Blurred vision and confusion
- Disorientation, speech difficulty
- Seizures or unconsciousness
- Sometimes death by insulin
Bottom line: Insulin is a prescription medication meant only for people who need it to manage diabetes. There is no safe or appropriate insulin dose for a non-diabetic person.
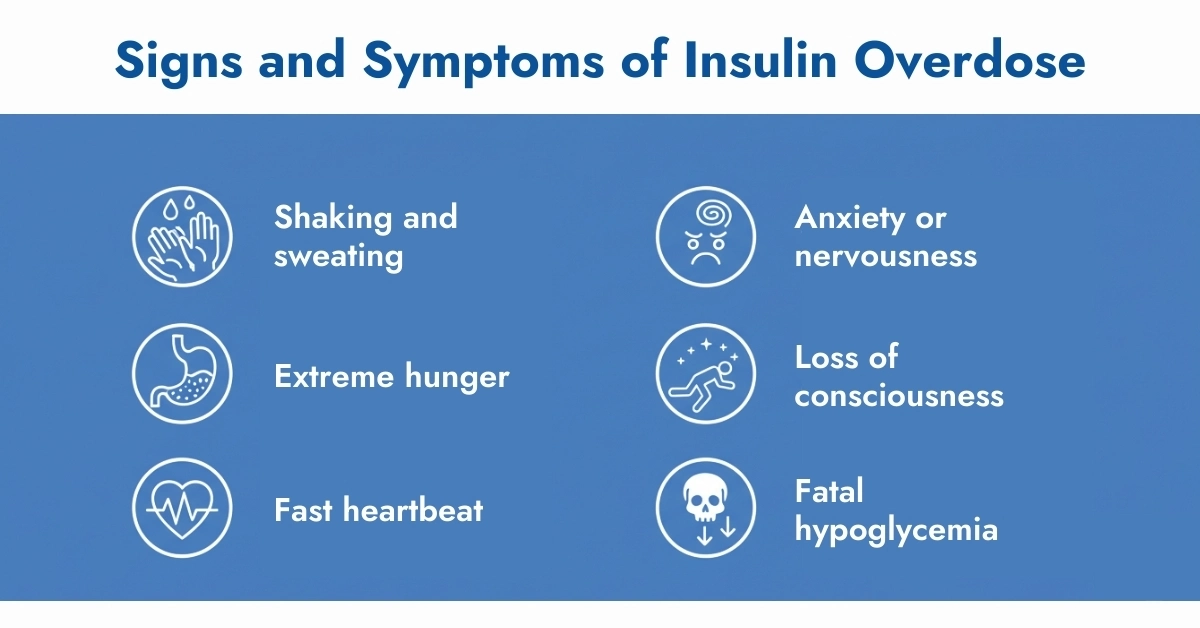
Signs and Symptoms of Insulin Overdose
Early Warning Signs
- Shaking and sweating
- Extreme hunger
- Fast heartbeat
- Anxiety or nervousness
Moderate to Severe Symptoms
- Difficulty speaking
- Blurred vision
- Seizures
- Unusual behavior or confusion
Life-Threatening Consequences
- Loss of consciousness
- Fatal hypoglycemia if untreated
- Brain damage from prolonged low blood sugar
Is There a Fatal Dose of Insulin for Non-Diabetics?
There is no safe insulin dose for a non diabetic person. What might be a routine dose for a diabetic patient can cause severe harm in a healthy person.
The fatal amount varies based on:
- Body weight and overall health
- Amount of glucose in the body at the time of injection
- Whether the person receives immediate treatment
Because of these unpredictable factors, any insulin injection in a non diabetic should be considered dangerous and potentially life-threatening.
What Should I do If Someone Injects Insulin By Mistake?
The result is a sudden drop in blood glucose if you take insulin without diabetes, with limited physiological defence. In many cases, individuals don’t realise how fast this drop occurs until symptoms turn dangerous. Here’s how to treat an insulin overdose immediately:
- 15-20g of glucose and a TruePlus tablet is a good option.
- Follow-up snack with protein and carbohydrates.
- Use the glucagon injection if available.
- Use Continuous glucose monitoring devices like FreeStyle Libre 3 Plus to prevent recurrence.
Emergency Treatment for Insulin Poisoning
If a non diabetic person accidentally or intentionally takes insulin, emergency medical help is required immediately.
First Aid Steps
- Consume fast-acting glucose such as sugar, juice, or glucose tablets if conscious.
- Never delay contacting emergency medical services.
Hospital Treatment
- Intravenous dextrose (IV sugar solution) to restore blood glucose.
- Emergency glucagon injection to counteract the insulin.
- Monitoring in an intensive care unit (ICU) to prevent further complications.
The poison control center should also be contacted for immediate advice while waiting for medical professionals.
Why Non-Diabetics Should Never Use Insulin
There are dangerous myths surrounding insulin use for:
- Weight loss
- Muscle building
- Performance enhancement
- Anti-aging
These practices are extremely unsafe and unsupported by medical science.
Important facts:
- Insulin is a prescription-only medication.
- Misuse can cause irreversible brain damage.
- Medication misuse is a leading cause of preventable medical emergencies.
Preventing Accidental Insulin Injections
Accidental use can happen in households where a family member uses insulin. To prevent mistakes:
- Store insulin in a labeled container away from children and non-diabetic adults.
- Educate family members about the dangers of taking insulin without diabetes.
- Regularly check your supply with guidance from your endocrinologist or diabetes educator
Real-Life Scenarios & Tools That Could Have Helped
Case 1: Ellen’s Mistake
In New York, Ellen Roger accidentally injected his roommate’s insulin pen, mistaking it for allergy medication. Within 15 minutes, he experienced dizziness, confusion, and began slurring words. His roommate acted fast with sugary drinks, and he survived. (Source: Cgm Monitors)
Case 2: Misuse After a Carb-Heavy Meal
A forum user admitted using 2 units of rapid insulin after eating a high-carb meal to “see how it worked.” An hour later, they were shaking, confused, and unable to speak clearly. It’s a harsh incident that occurred to him.
Death by Insulin: A Worst Scenario Ever
Death by insulin is not hypothetical; medical journals confirm fatalities, especially in non-diabetics. Documented cases include accidental injections, depression-related suicides, and even homicides, such as nurse Colin Norris, convicted for using insulin as a weapon. A study in the National Library of Medicine outlines insulin-induced hypoglycemia deaths in non-diabetics. Therefore, insulin must be stored securely and used under supervision only.
Conclusion
Overall, death by insulin is real, but it’s easily preventable as long as you have glucose intake within reach. Never use insulin for weight gain, loss, wound healing, or anti-ageing, as there is less scientific backing for all of them. Using insulin as a non-diabetic can result in coma, seizures, or fatal hypoglycemia. Even small amounts can trigger critical drops in blood glucose. This is why continuous glucose monitors (CGMs) are handy, as they detect drops in real time. Tools like the Dexcom G7 Receiver are not just for diabetics; they offer real-time safety insight. For anyone managing insulin exposure, CGMs serve as a vital safeguard. When in doubt, treat and call for help.
Frequently Asked Questions
What are the long-term side effects of insulin use in non-diabetics?
Long-term side effects include insulin resistance, electrolyte imbalance, cognitive decline, and in older adults, falls or heart strain.
Can a small amount of insulin harm a non-diabetic?
Yes. Even small amounts can cause dangerous drops in blood sugar.
Is insulin poisoning reversible?
If treated quickly with glucose, recovery is possible. Delayed treatment increases the risk of brain injury or death.
Can I use insulin to lose weight?
No. It’s dangerous, unsupervised, and can lead to weight gain from rebound sugar consumption or severe hypoglycemia.
Can an insulin overdose cause a heart attack?
Not directly, but severe hypoglycemia may increase cardiovascular stress, especially in older or at-risk individuals.
What should I do if I accidentally inject insulin?
Eat fast carbs immediately ( glucose tablets) and seek medical attention, delays are dangerous.
Can small doses of insulin harm a non-diabetic?
Yes. Even 1-2 units can cause hypoglycemia, especially if fasting or without medical supervision.
Is there an antidote for insulin overdose?
Yes, glucose is the first-line treatment. Severe cases may need intravenous dextrose in a hospital.
Why would a non-diabetic use insulin?
Some misuse it for weight loss or performance. These practices are high-risk and medically unsound.
Is it possible to kill someone with insulin without leaving traces?
Yes. Per Wiley Forensic Review, insulin deaths are hard to detect postmortem due to rapid metabolism and nonspecific symptoms.



Write a comment
Your email address will not be published. All fields are required