Table of content
- What Is Compression Therapy?
- How Compression Therapy Supports Circulation
- Common Uses of Compression Therapy
- Medical Conditions Treated With Compression Therapy
- Types of Compression Therapy Devices
- Top Benefits of Compression Therapy
- Final Thoughts: Is Compression Therapy Right for You?
- Frequently Asked Question
Compression therapy is a clinically proven treatment approach widely used to improve blood circulation, reduce swelling, and support vascular and lymphatic health. From managing chronic venous disorders to post-surgical recovery and lymphedema care, compression garments and pneumatic compression play a critical role in preventive healthcare.
In this comprehensive guide, we’ll explain how compression therapy works, its medical and clinical uses, conditions it treats, and the different types of compression therapy devices, including advanced solutions like the Biocompression Pump.
What Is Compression Therapy?
Compression therapy is the process of applying controlled external pressure with the help of garments to the skin and other tissues with biocompression garments or devices. The pressure assists in narrowing blood vessels. This accelerates the flow of blood venous and also reduces the pooling of blood in the legs.
The primary goal of compression therapy is to:
- Improve venous return
- Reduce fluid buildup (edema)
- Prevent blood pooling
- Support tissue healing
Compression therapy is commonly prescribed by physicians, vascular specialists, wound care clinics, and physical therapists. The top most favourite pneumatic compression stock are available on our BioCompression Category. You can check here.
How Compression Therapy Supports Circulation
The Science Behind Compression Therapy
Compression therapy works by applying graduated or intermittent pressure to the affected area. This pressure narrows vein diameter, which helps:
- Push blood back toward the heart
- Improve valve function in veins
- Reduce venous reflux
- Stimulate lymphatic drainage
Key Mechanisms:
- Improved circulation: Prevents blood from pooling in extremities.
- Reduced swelling: Moves excess fluid out of tissues.
- Pain relief: Decreases pressure on nerves and tissues.
- Faster healing: Enhances oxygen and nutrient delivery.
In advanced systems like pneumatic compression pumps, pressure cycles mimic natural muscle contractions, making them highly effective for chronic conditions.
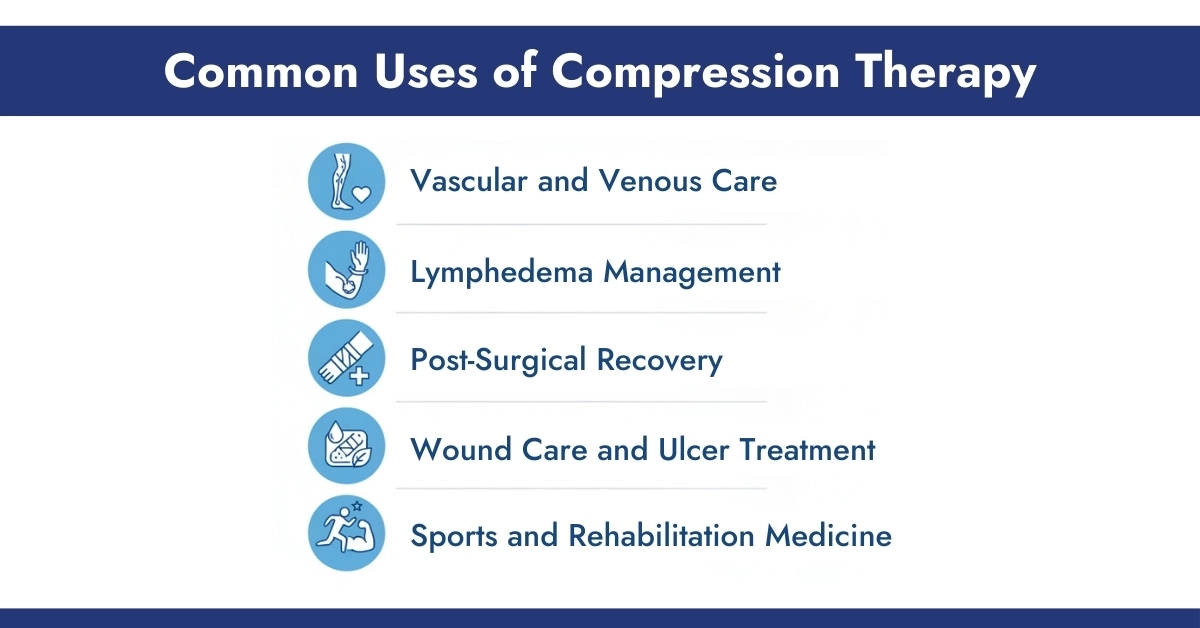
Common Uses of Compression Therapy
Compression therapy is used across multiple medical specialties and care settings.
1. Vascular and Venous Care
- Improves venous insufficiency
- Prevents varicose vein progression
- Reduces leg heaviness and fatigue
2. Lymphedema Management
- Helps move lymph fluid
- Prevents tissue fibrosis
- Maintains limb volume reduction
3. Post-Surgical Recovery
- Reduces post-operative swelling
- Lowers risk of blood clots (DVT)
- Enhances healing after orthopedic or vascular surgery
4. Wound Care and Ulcer Treatment
- Supports healing of venous leg ulcers
- Improves outcomes in chronic wound clinics
5. Sports and Rehabilitation Medicine
- Accelerates muscle recovery
- Reduces inflammation and soreness
- Improves athletic performance recovery
Advanced pneumatic devices like the Bio Compression SC-4008-DL and SC-2008-DL offer adjustable sequential pressure up to 100 mmHg. These systems are ideal for post-surgical lymphatic drainage, chronic edema, and lymphedema care at home. Choosing the right compression device depends on your medical need, mobility level, and treatment goals.
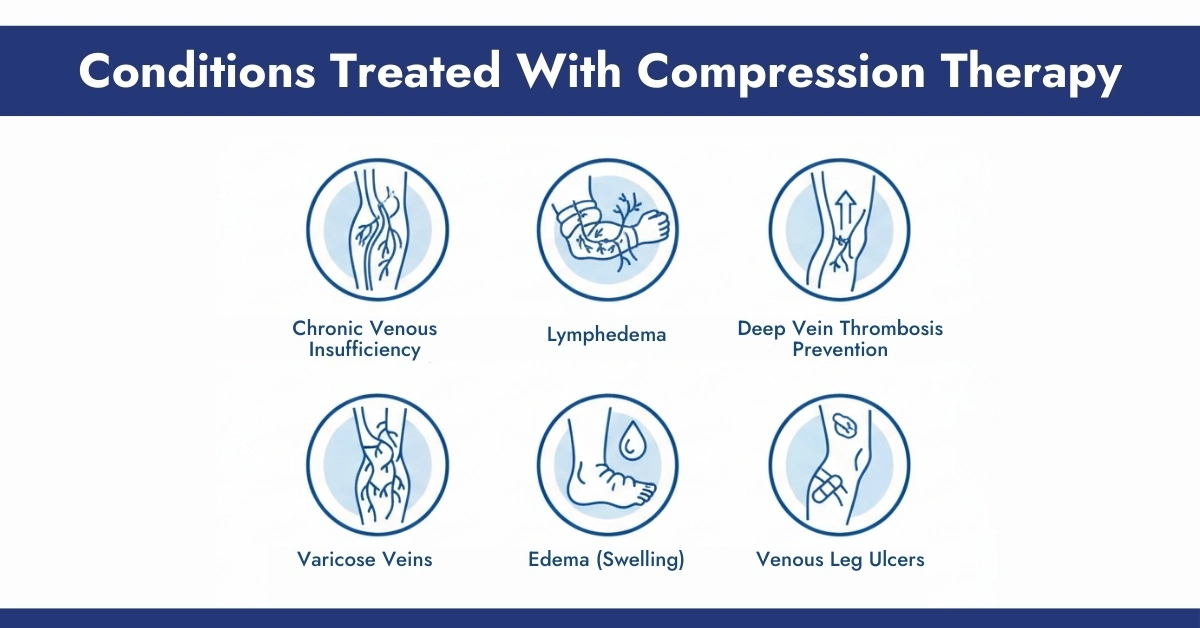
Medical Conditions Treated With Compression Therapy
Chronic Venous Insufficiency (CVI) – A condition where veins struggle to return blood to the heart, causing swelling, pain, and skin changes.
Lymphedema – A chronic condition involving lymph fluid buildup, often after cancer treatment or surgery. BioCopression pumps very helpful in this condition.
Deep Vein Thrombosis (DVT) Prevention – Compression helps reduce clot risk during prolonged immobility or hospitalization.
Varicose Veins – Compression minimizes vein enlargement and relieves discomfort.
Edema (Swelling) – Caused by heart failure, pregnancy, injury, or prolonged sitting/standing.
Venous Leg Ulcers – Compression is a gold-standard therapy in wound care protocols.
Types of Compression Therapy Devices
Understanding the available compression therapy devices helps both patients and clinicians select the most effective solution based on medical condition, severity, and care setting.
1. Compression Stockings and Garments
Compression stockings and garments are the most commonly prescribed form of compression therapy and are typically used as a first-line treatment. They apply graduated compression, with higher pressure at the ankle that gradually decreases upward, promoting efficient blood flow back to the heart. Available in knee-high, thigh-high, and full-length options, these garments usually deliver pressure levels ranging from 8–30+ mmHg.
2. Pneumatic Compression Devices
Pneumatic Compression Devices use air-filled chambers that inflate and deflate in programmed cycles to actively move blood and lymphatic fluid. These devices are especially beneficial for patients with lymphedema, chronic swelling, and post-surgical fluid retention.
3. Biocompression Pumps
The Biocompression Pump is an advanced form of pneumatic compression therapy designed to deliver sequential, gradient pressure through multi-chamber garments like 8 Chamber Bio Abdominal Sleeve. It closely mimics the body’s natural lymphatic and venous flow, making it highly effective for managing lymphedema and chronic swelling. Biocompression pumps improve treatment outcomes, increase patient compliance, and are safe for home use when prescribed and monitored by a healthcare provider.
Top Benefits of Compression Therapy
- Vascular Health and Circulation – Leg compression therapy can alleviate the symptoms associated with chronic venous impairment. It helps maintain the function of the vein valve and decreases the risk of developing vein ulcers.
- Edema Reduction and Ulcer Healing – Compression is a way to control the flow of fluid into soft tissues, a major factor in edema and wounds that are not healing.
- Athletic Recovery – Athletes wear air-compression footwear after exercise to ease soreness and speed up the recovery of muscles. IPC devices assist in clearing lactic acid and enhancing oxygenation of the muscles.
- Everyday Support – Nurses, frequent flyers, seniors, and pregnant individuals benefit from consistent use. Compression helps reduce leg fatigue, prevents fluid pooling, and supports better energy levels during long shifts or flights.
Final Thoughts: Is Compression Therapy Right for You?
Compression therapy is a cornerstone treatment for vascular, lymphatic, and post-surgical conditions. Whether through simple compression stockings or advanced systems like the Biocompression Pump, this therapy offers reliable, evidence-based relief when used correctly.
For patients dealing with chronic swelling, venous disease, or lymphedema, compression therapy that is guided by clinical expertiss, can significantly improve daily comfort, mobility, and long-term health outcomes.
Frequently Asked Question
Do compression boots work?
Yes, User feedback and studies confirm that the intermittent pneumatic compression decreases swelling and speeds recovery.
Are leg compression massagers good for you?
Yes. When used with proper settings and frequency, they reduce fatigue and fluid buildup.
Is compression therapy safe for diabetics?
Yes. Many DFUs respond well to therapeutic compression, even with mild arterial impairment.
What are air compression boots used for?
They help reduce DOMS, promote venous return, and prevent DVT in immobile patients.
Are compression boots worth it?
For patients with issues with circulation or recovery requirements or a long-term swelling the long-term benefits outweigh the initial cost.





Write a comment
Your email address will not be published. All fields are required