Table of content
Cystic Fibrosis Diabetes (CFRD) is a unique and often overlooked complication that affects many individuals living with cystic fibrosis (CF). Unlike traditional forms of diabetes, CFRD combines features of both Type 1 and Type 2 diabetes and presents distinct challenges due to the underlying condition. For those managing CFRD, consistent blood sugar monitoring is essential, and modern Continuous Glucose Monitoring (CGM) devices provide an invaluable tool to help patients maintain better control.
In this article, we’ll explore what CFRD is, how it develops, its symptoms, and most importantly, how CGM devices can transform the way cystic fibrosis patients manage their blood sugar.
Understanding Link Between Cystic Fibrosis and Diabetes
Cystic fibrosis is a genetic condition stemming from CFTR gene mutations that impact the lungs, pancreas, and other organs. A key complication is pancreatic insufficiency, impairing enzyme production for digestion and insulin for blood sugar control. This eventually results in insulin deficiency and Cystic Fibrosis-Related Diabetes (CFRD).
Distinct from Type 1 diabetes, which involves autoimmune damage to insulin-producing cells, or Type 2 diabetes, driven mainly by insulin resistance, CFRD combines both deficiency and resistance. This hybrid nature complicates blood sugar monitoring. Grasping these differences is essential for effective treatment.
Why Does Cystic Fibrosis Lead to Diabetes?
Insulin production is the most important function of the pancreas. The very dense mucus that typifies the disease CF can clog the ducts of the pancreas. This would prevent the digestive enzymes from passing to the intestines to facilitate digestion. Inflammation can set in while food stays in one place. Over time, the inflammation can damage the cells of the pancreas that produce insulin.
This leads to insulin deficiency or insulin resistance, thus raising the sugar level in the blood. The condition is called cystic fibrosis diabetes.
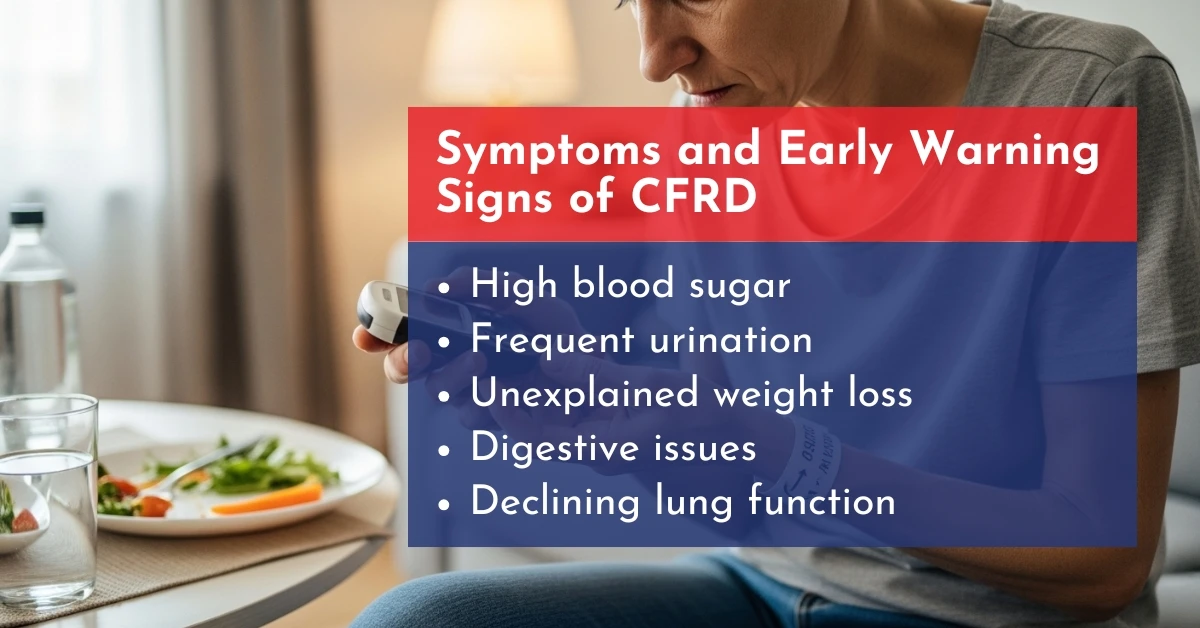
Symptoms and Early Warning Signs of CFRD
Early detection of CFRD is vital because symptoms can be subtle or attributed to cystic fibrosis itself. Common signs include:
- High blood sugar (hyperglycemia)
- Frequent urination and increased thirst
- Fatigue and low energy levels
- Unexplained weight loss despite adequate nutrition
- Digestive issues and poor nutrient absorption
- Declining lung function, as high blood sugar can worsen respiratory health
Because CF already affects metabolism and lung function, early monitoring using CGM devices can alert patients to fluctuating blood sugar levels before complications develop.
Diagnosis of Cystic Fibrosis Diabetes
The diagnosis of CFD is usually made with the aid of any or all of the following methods:
- For Blood Glucose Tests: Doctors use either a fasting blood glucose test or an oral glucose tolerance test (OGTT) to check blood sugar and detect diabetes.
- Hemoglobin A1c Test: This is an average of the levels of blood sugar over the last two to three months, giving facts regarding long-term blood sugar control.
- Continuous Glucose Monitoring: Patients may wear a continuous glucose monitor to record their blood glucose levels throughout the day and night.
Screening for CFD, through routine measures, is a must for all patients with CF. Since it is a significant comorbidity with cystic fibrosis, an early diagnosis will enhance the chances of improved management. On the other hand, managing cystic fibrosis-related diabetes is complex because it involves all the challenges of diabetes along with additional disorders associated with cystic fibrosis.
Managing CFRD: Lifestyle and Medical Approaches
Managing Cystic Fibrosis-Related Diabetes (CFRD) involves a comprehensive approach, integrating insulin therapy, dietary adjustments, and lifestyle changes.
1. Insulin Therapy
Insulin is the cornerstone of CFRD treatment, addressing insulin deficiency from pancreatic damage. Unlike Type 2 diabetes, oral medications are typically insufficient. Regular monitoring with Continuous Glucose Monitoring (CGM) devices guides precise dosing to maintain stable blood sugar and prevent extreme fluctuations.
2. Nutrition and Diet
A balanced diet tailored for cystic fibrosis and diabetes is crucial. Patients require sufficient calories for lung function while controlling blood sugar. Focus on:
- Whole grains
- Low-glycemic index foods
- Healthy fats (e.g., avocados)
- Proper hydration
Avoiding rapid blood sugar spikes reduces hyperglycemia risks. CGM devices help patients monitor how foods affect glucose levels in real time.
3. Exercise and Physical Activity
Regular exercise enhances insulin sensitivity and supports health. Activities like walking, swimming, or CF-appropriate workouts stabilize blood sugar and improve lung function.
4. Pancreatic Support
Pancreatic Enzyme Replacement Therapy (PERT) is often necessary for CF patients to improve digestion and nutrient absorption, indirectly aiding glucose control and overall health.
5. Stress Management and Lifestyle
Stress can raise blood sugar, particularly in CFRD patients with variable glucose levels. Mindfulness, adequate sleep, and hydration are vital. CGM devices help identify how stress or activity impacts glucose patterns.
Preventing Complications in CFRD
Stable blood sugar control is essential in Cystic Fibrosis-Related Diabetes (CFRD) to avoid long-term issues like kidney damage, nerve damage, and declining lung function.
Practical Tips:
- Adopt a CFRD-friendly diet rich in low-glycemic foods.
- Maintain proper hydration to aid glucose regulation.
- Schedule regular visits with endocrinologists and CF specialists.
- Utilize Continuous Glucose Monitoring (CGM) devices like FreeStyle Libre 2 plus or Simplera Sync to track trends and adjust insulin or lifestyle as needed.
Proactive management supports lung health, weight stability, and overall well-being.

Conclusion
Cystic Fibrosis-Related Diabetes (CFRD) demands vigilant blood sugar control, nutrition, and wellness. Continuous Glucose Monitoring (CGM) devices provide real-time tracking, complication prevention, and enhanced healthcare collaboration.
For those managing CFRD, incorporating CGM into routines boosts control, eases stress, and fosters well-being. Discover our CGM solutions tailored for cystic fibrosis patients to monitor and regulate blood sugar efficiently.
Frequently Asked Questions
What is the difference between CFRD and Type 1 or Type 2 diabetes?
CFRD involves both insulin deficiency due to pancreatic damage and some insulin resistance, unlike Type 1 diabetes, which is caused by autoimmune destruction of insulin-producing cells, or Type 2 diabetes, which is primarily driven by insulin resistance.
How often should a CFRD patient check their blood sugar?
Continuous Glucose Monitoring (CGM) devices allow ongoing tracking, but fingerstick tests may be needed periodically to calibrate the device and ensure accuracy.
Can diet alone manage CFRD?
No, diet is important but insufficient alone. Insulin therapy and consistent monitoring are typically required for effective management.
How do CGM devices help prevent complications in CFRD?
CGM devices provide real-time glucose readings and alerts for high or low levels, helping patients make timely adjustments to avoid complications like kidney or nerve damage.
Are there specialized CGM devices for cystic fibrosis patients?
Many CGM devices are suitable for CFRD, offering features like trend alerts and remote monitoring, though none are exclusively designed for cystic fibrosis patients.











Write a comment
Your email address will not be published. All fields are required