Table of content
- Understanding Ketoacidosis — The Basics
- What is Starvation Ketoacidosis?
- Symptoms of Starvation Ketoacidosis
- Treatment for Starvation Ketoacidosis
- What is Diabetic Ketoacidosis (DKA)?
- Who is at Risk?
- Preventing Ketoacidosis — Key Tips
- User Experience: What to Do if You Suspect Ketoacidosis
- Conclusion
- Frequently Asked Questions
Maintaining healthy blood sugar and metabolism is a delicate balance, controlled by what we eat, how much energy we burn, and how well our body uses insulin. When that balance is disrupted, the body can enter a dangerous state known as ketoacidosis.
Two of the most common types — Starvation Ketoacidosis and Diabetic Ketoacidosis (DKA) — may sound similar, but their causes, symptoms, and treatments are quite different. Understanding these differences is vital to prevent life-threatening complications.
Understanding Ketoacidosis — The Basics
Before diving into the differences, it’s essential to understand what ketoacidosis is.
In simple terms, ketoacidosis occurs when the body starts breaking down fats for energy because it doesn’t have enough glucose (sugar). This process produces ketone bodies, acidic compounds that, in large amounts, can make the blood dangerously acidic — a condition known as metabolic acidosis.
While ketosis (like in low-carb diets) is usually safe and mild, ketoacidosis is a medical emergency that requires prompt treatment. There are different types of ketoacidosis — the most notable being diabetic ketoacidosis and starvation ketoacidosis.
What is Starvation Ketoacidosis?
Starvation Ketoacidosis occurs when the body is deprived of food for a prolonged period — typically several days — and glucose stores become depleted. With no incoming carbohydrates, the liver begins converting fat into ketones for energy. In short-term fasting, this is normal. But when starvation continues, ketone body production increases to dangerous levels, causing ketoacidosis.
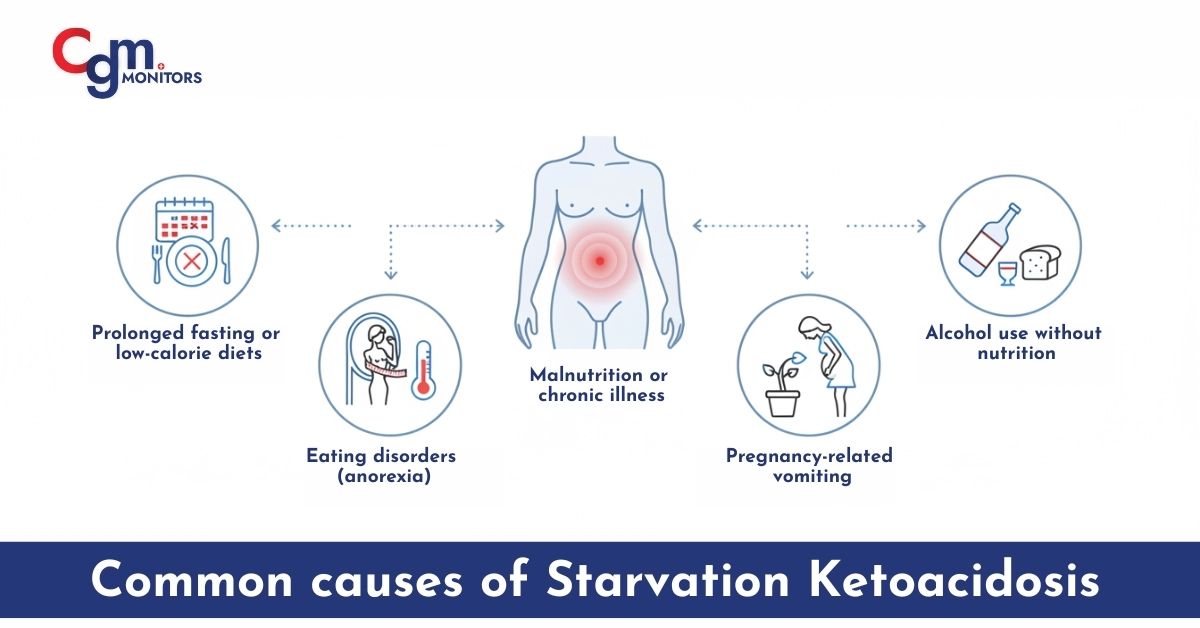
Common causes of starvation ketoacidosis include:
- Prolonged fasting or very low-calorie diets
- Eating disorders like anorexia nervosa
- Malnutrition or chronic illness
- Pregnancy-related nausea and vomiting
- Alcohol use without adequate nutrition
This condition can occur even in non-diabetic individuals, making it an often overlooked cause of metabolic acidosis in emergency settings.
Symptoms of Starvation Ketoacidosis
Symptoms may appear mild initially but can worsen quickly if untreated. Common symptoms of starvation ketoacidosis include:
- Nausea and vomiting
- Fatigue and confusion
- Rapid breathing (Kussmaul respirations)
- Dehydration due to fluid loss
- Fruity or acetone-like breath odor
Also, physical clues of starvation: muscle wasting, pale skin, low pulse, and even dental and hair changes.
Treatment for Starvation Ketoacidosis
Treatment focuses on restoring nutrition and reversing acidosis. Doctors usually administer IV fluids containing glucose to provide immediate energy, reduce fat breakdown, and stop ketone production. In some cases, electrolyte correction and thiamine supplementation are needed to prevent complications.
Reintroducing nutrition — known as refeeding — must be done carefully to avoid refeeding syndrome, a condition where sudden nutrient intake causes severe electrolyte imbalance.
What is Diabetic Ketoacidosis (DKA)?
Diabetic Ketoacidosis is a more severe and well-known form of ketoacidosis that occurs primarily in people with Type 1 Diabetes, though it can also affect those with Type 2 Diabetes under stress, infection, or poor insulin control. In DKA, the lack of insulin prevents glucose from entering the body’s cells. The body mistakenly thinks it’s starving and starts breaking down fat for energy, leading to a buildup of ketone bodies and acidic blood pH.
Common causes of diabetic ketoacidosis include:
- Insulin deficiency or missed doses
- Infections or illnesses that increase glucose levels
- Uncontrolled diabetes
- High stress or injury
- Alcohol or drug use in diabetics
Symptoms of Diabetic Ketoacidosis
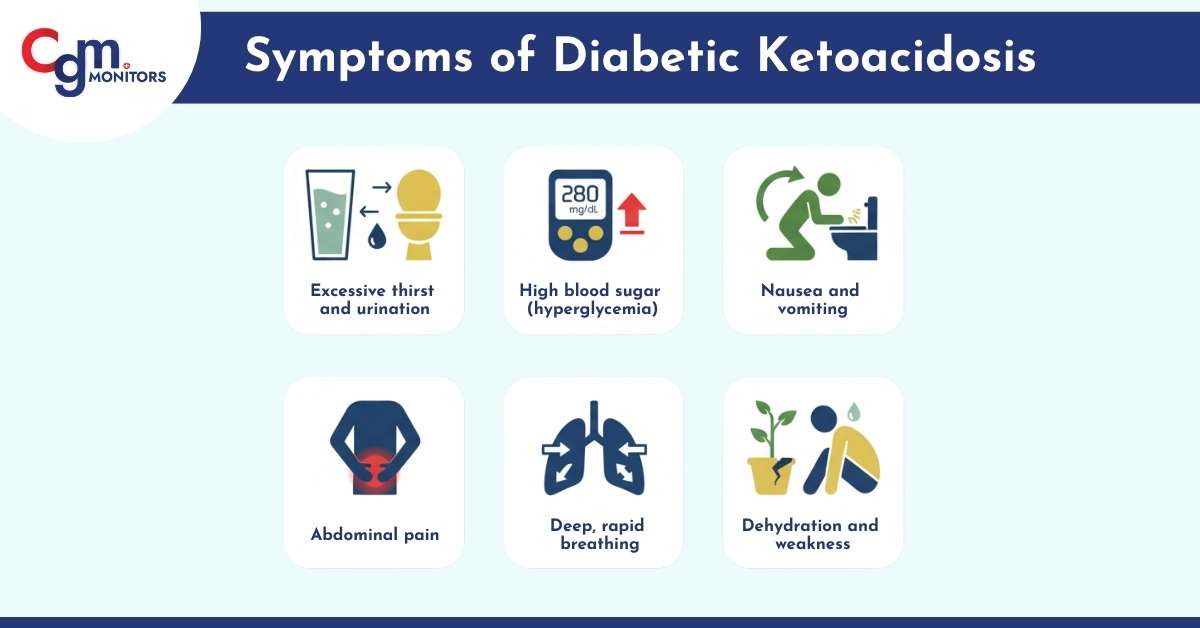
The symptoms of diabetic ketoacidosis often develop rapidly, within hours. They include:
- Excessive thirst and urination
- High blood sugar (hyperglycemia)
- Nausea and vomiting
- Abdominal pain
- Deep, rapid breathing
- Dehydration and weakness
- Fruity-smelling breath
- Confusion or even coma in severe cases
If untreated, DKA can progress to shock, organ failure, or death — making early intervention critical.
Treatment and Management of DKA
The treatment of diabetic ketoacidosis is typically hospital-based and involves:
- IV insulin therapy to stop ketone production and lower blood sugar
- IV fluids to treat dehydration
- Electrolyte correction (especially potassium)
- Monitoring of blood pH, glucose, and ketone levels
Once stable, patients are transitioned back to subcutaneous insulin and educated on diabetes management to prevent recurrence.
Who is at Risk?
Starvation Ketoacidosis can affect anyone undergoing prolonged fasting or restrictive dieting. Pregnant women with severe morning sickness, people with eating disorders, or those on extreme low-carb regimens are especially at risk.
On the other hand, Diabetic Ketoacidosis primarily affects people with Type 1 Diabetes, but it can also occur in Type 2 diabetics during stress, infections, or insulin non-compliance.
Both forms of ketoacidosis require urgent medical attention.
Did you know?
Dexcom G7 sensors give alerts about 15 minutes before your sugar levels go down. Get a free benefits check with CGM Monitors today.
Preventing Ketoacidosis — Key Tips
To prevent Starvation Ketoacidosis:
- Avoid extreme fasting or restrictive diets—especially unsupervised keto + fasting
- If you’re dealing with eating disorders or malnutrition, talk to a professional
- Gradual refeeding is key—don’t binge or add calories too fast
- Stay hydrated & monitor nutrition carefully

To Prevent Diabetic Ketoacidosis:
- Monitor blood sugar regularly
- Never skip insulin doses
- Stay hydrated and manage stress
- Seek prompt treatment for infections
- Use continuous glucose monitors (CGMs) like Dexcom G6 or Freestyle Libre 3 Plus for better control.
User Experience: What to Do if You Suspect Ketoacidosis
If you experience nausea, vomiting, rapid breathing, or confusion, and especially if you have diabetes or have been fasting, seek emergency medical attention immediately.
Testing for blood glucose and ketone levels can help identify whether it’s starvation ketoacidosis or diabetic ketoacidosis.
In hospital settings, doctors perform blood pH, bicarbonate, and glucose tests to confirm the diagnosis.
Early diagnosis ensures faster recovery and prevents complications like kidney damage or brain swelling.
Conclusion
Both Starvation Ketoacidosis and Diabetic Ketoacidosis are serious metabolic emergencies with overlapping symptoms but distinct causes. While starvation ketoacidosis results from prolonged fasting and low glucose intake, diabetic ketoacidosis stems from insulin deficiency and high blood sugar.
Recognizing the symptoms of ketoacidosis, seeking early treatment, and maintaining proper nutrition or diabetes control can save lives. Whether you’re fasting, dieting, or managing diabetes, the key lies in balance, awareness, and timely medical care.
Disclaimer: This blog is for informational purposes only and does not constitute medical, legal, or professional advice. While we strive for accuracy, errors or omissions may occur.
Frequently Asked Questions
Can a low-carb or ketogenic diet cause ketoacidosis?
Normally, a low-carb or keto diet causes nutritional ketosis, not ketoacidosis. It becomes risky only with severe calorie restriction or dehydration.
Can starvation ketoacidosis occur during pregnancy?
Yes. It can happen during prolonged vomiting or poor intake and needs prompt medical attention.
How long does it take to develop diabetic ketoacidosis (DKA)?
DKA can develop within a few hours to a day, especially if insulin is missed or during illness.
Can someone have diabetic ketoacidosis with normal blood sugar levels?
Yes. This is called Euglycemic DKA, often linked to certain diabetes medications or fasting.
What happens if ketoacidosis is left untreated?
Untreated ketoacidosis can lead to severe dehydration and organ damage, requiring emergency care.
Can both starvation and diabetic ketoacidosis occur together?
Yes. A diabetic person who is also fasting or not eating properly can experience both at once.
Can alcohol use trigger ketoacidosis?
Yes. Heavy alcohol use without food can lead to alcoholic ketoacidosis, a condition similar to starvation ketoacidosis.



Write a comment
Your email address will not be published. All fields are required